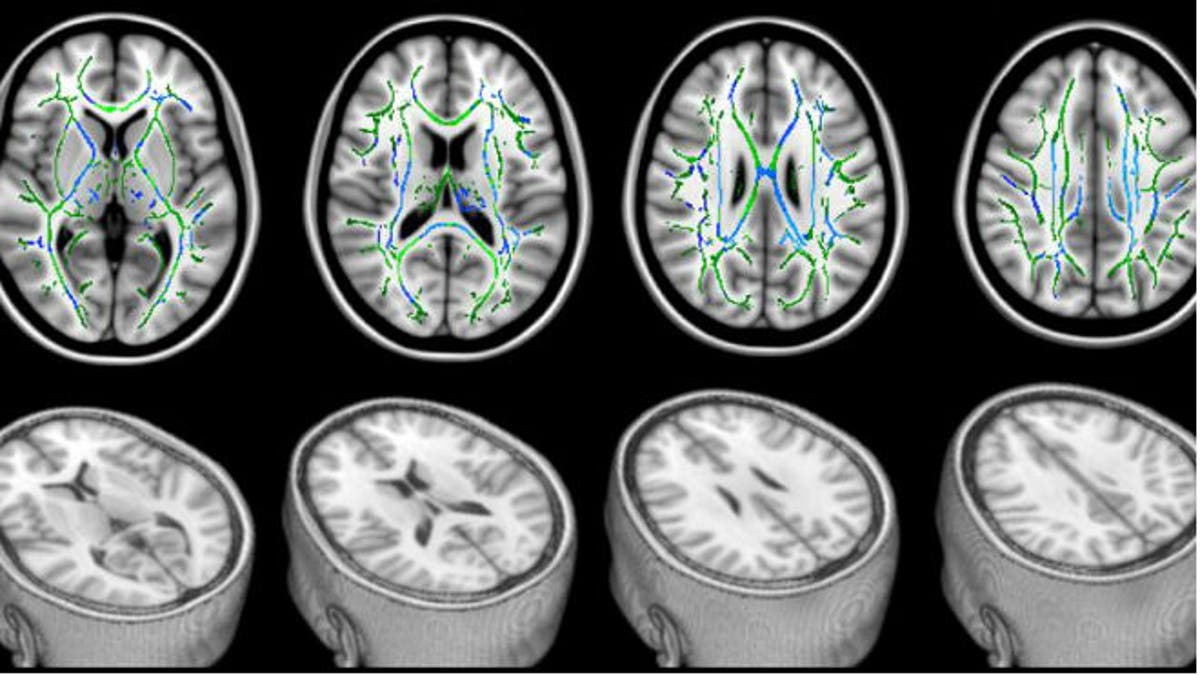
In these DTI scans, the bottom row shows views of a head with the top sliced away to reveal the brain. The top row shows the corresponding top views of the brain. The green lines represent the white matter— the brain’s “wiring.” The blue areas are the damaged parts of the white matter that seem to be responsible for cognitive problems experienced by study patients with mild traumatic brain injury. (Professor Blamire/Newcastle University, UK)
While much is known about the effects of severe traumatic brain injuries (TBI), less attention has been paid to mild and moderate brain injuries.
In a new study published in Neurology, researchers have found that mild TBI may impact patients’ cognition and brain matter.
“The [study’s] focus was really on the mild end… because they’re by far the biggest group of patients when looking at TBI breakdowns— 90 percent of patients have mild to moderate injuries,” study author Andrew Blamire, a professor of magnetic resonance physics at Newcastle University in the United Kingdom, told FoxNews.com. “In terms of trying to understand what happens to the brain immediately after injury, many of these individuals will have cognitive problems… there’s no way of working out which of these will have ongoing problems.”
To address this issue of identifying those with brain damage after injury, researchers at Newcastle University used diffusion tensor imaging (DTI), a method of magnetic resonance imaging (MRI) that is routinely used for acute ischemic stroke and severe trauma. DTI images use contrast and brightness to determine the health of brain tissue. In a healthy brain, the brain’s white area— the interconnected wiring between different brain areas— is very structured and orderly. If there is damage to the cellular structure of the brain, the DTI image shows changes in the brightness of the image.
Working with a group of 44 people with mild TBI, nine people with moderate TBI and a control group of 33 healthy participants— who were closely matched by age and education level with individual patients— researchers administered DTI scans within one week of injury and used the Glasgow Coma Scale (GSC) test to measure cognition.
The GSC test analyzes a patient’s responsiveness in three areas: eye movement, verbal activity and general movement. A patient with a GCS number between 12 to 15 is considered to have a mild injury; a fully responsive person would score a 15. A score below nine is indicative of a severe injury.
Researchers found that, compared to the control group, participants with brain injuries had DTI scans showing damage to the brain’s white matter. The brain’s white matter is the “wiring” between the key areas in the brain, including cognitive processes of language and memory.
“Damage to that interconnection could mean it affects a whole range of functions; it’s complicated to know precisely what they all do,” Blamire said.
Additionally, injured particpants’ GCS test scores were 25 percent lower than the healthy participants. People who have mild TBI—which can include having a concussion or being briefly unresponsive or less responsive than normal— may not be aware that they’re dealing with cognitive side effects. Scans showed that the bigger the brain changes in a particular individual, the worse they performed on tests of verbal fluency.
“There’s a very strong relationship to how badly you were affected in terms of cognitive function, and how badly your brain seemed to be altered as a result of the injury on the MRI scan,” Blamire said.
In a 12-month follow up, most of the patients’ cognitive function had improved, but their brain scans showed some areas had returned to normal while others hadn’t. Blamire noted that after one year, any damage done to the brain is generally considered to be permanent. However, because the brain is so elastic, it may rewire itself to create a coping strategy, which may explain the sustained damage at 12 months, but the improved cognitive function, he said.
Blamire called the study and its use of DTI a first step to better understanding and treating mild TBI that includes better educating clinicians, targeting intervention and improving recovery. DTI is an unconventional scanning method for mild injuries, but, combined with GCS testing, may be better at properly identifying injured patients than traditional MRI or computerized tomography (CT) scans.
“[DTI] reveals the true level and extent of injury for the first time,” Blamire said. “It goes toward helping understand the relationship between the clinical status of a patient and what’s happening to the brain in a way that we haven’t been able to do before.”







































