Middle East respiratory syndrome (MERS) is spreading in South Korea, with dozens of people there infected and thousands more under quarantine because they have had contact with an infected person, according to news reports.
But although the virus could certainly arrive on U.S. soil, it is highly unlikely to spread widely here, one expert says.
That's because it's fairly easy to prevent MERS transmission, once doctors realize they are dealing with the virus, said Dr. Amesh Adalja, an infectious-disease physician at the Center for Health Security at the University of Pittsburgh.
Most doctors in the United States know to take a travel history and isolate people who may harbor a dangerous virus, which are key steps in stopping transmission in its tracks, he said. And MERS doesn't spread readily in the community, Adalja added. [8 Things You Should Know About MERS]
Camel-based virus
So far, at least 87 people in South Korea have become infected with MERS, and six of those people have died. At least 1,870 schools have been closed, and thousands of people are under quarantine after exposure to patients with the virus, according to the Los Angeles Times.
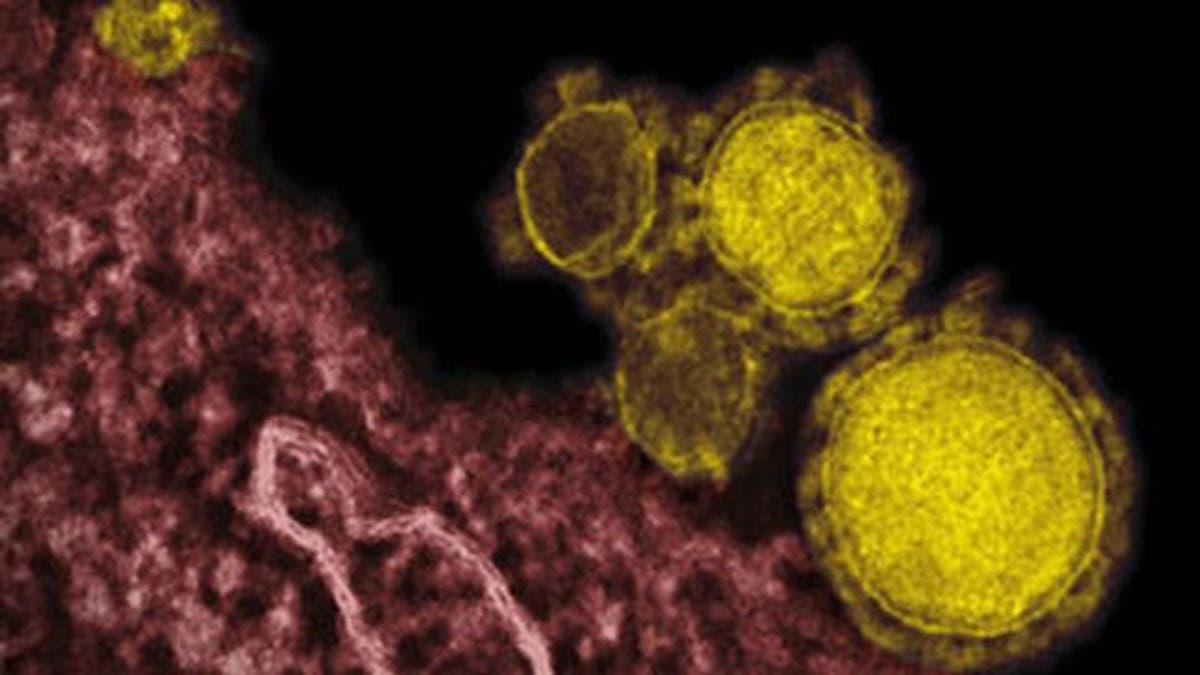
The virus that causes MERS, which first emerged in Saudi Arabia in 2012, is part of the family of viruses that includes the one that causes the common cold. Doctors now believe that bats were the original hosts for the pathogen, which jumped from bats to camels. People who have close contact with camels, such as shepherds, can sometimes become infected.
Like the common cold, the MERS-coronavirus causes coughing, sneezing and other respiratory symptoms. However, the disease can also cause pneumonia and kidney failure, and can be deadly.
It's unclear exactly how deadly the virus may be, Adalja said. Previous studies have found that the virus may kill up to 38 percent of people infected with it, but scientists now think the disease may not be so deadly. In addition, experts say the number of people infected with the virus may have been underestimated because some people did not seek health care.
"We're seeing the tip of the iceberg — we're seeing the people who are diagnosed," Adalja said. A 2014 study in the journal The Lancet that looked at 10,000 people in Saudi Arabia found that many people had antibodies to the virus, meaning they had been exposed to it and either didn't show any symptoms or had not been diagnosed with MERS.
That finding suggests the disease course may be milder than the diagnosed cases seem to indicate, Adalja said.
Hard to catch
In addition, the disease does not spread readily between humans. In one study, just 12 of the 280 family members who lived in the same homes as MERS patients developed antibodies to the disease, and most of those people developed only very mild symptoms.
"We haven't seen the ability of the virus to spread in the community," Adalja told Live Science.
In the current outbreak, human-to-human transmission has so far taken place largely in hospital settings, where infection control was inadequate, Adalja said.
In South Korea, for instance, a few dozen cases were tied to the first patient, who was admitted to St. Mary's Hospital in Pyeongtaek, outside of Seoul, before doctors realized that he had MERS. The reason the virus may have been able to pass from this "superspreader" patient to so many others was that the man was receiving oxygen-based treatments, which could have aerosolized the virus particles and enabled them to spread through the hospital ward, Adalja said. All of the South Korean cases are tied to 24 hospitals, and only six of those hospitals had person-to-person transmission inside the hospital, The New York Times reported.
Stepped-up response
Now that the South Korean government is on high alert, it is taking the right steps to halt the disease, Adalja said. Not only are hospitals appropriately isolating suspicious patients, but they are now quarantining all of the people who have come into contact with those patients, tracking their movements via cellphone towers to make sure they are adhering to the quarantine, South Korea's deputy prime minister, Choi Kyung-hwan, said at a news conference Sunday.
The United States is equipped to handle any cases of MERS that do show up, Adalja said. There were two people who became sick with MERS in the U.S. after traveling here from the Middle East last year, and neither of those patients spread the disease, Adalja said.
The first step in stopping the virus' spread is to take a thorough travel history, Adalja said. People with respiratory symptoms who have been in the Middle East in the past two weeks should be isolated appropriately, he said.
Because of the ongoing Ebola outbreak, many doctors and first-line responders in the U.S. have already received additional training on how to take a travel history and be alert for potential cases, he added.
- The 9 Deadliest Viruses on Earth
- 10 Deadly Diseases That Hopped Across Species
- 5 Viruses That Are Scarier Than Ebola
Copyright 2015 LiveScience, a Purch company. All rights reserved. This material may not be published, broadcast, rewritten or redistributed.
