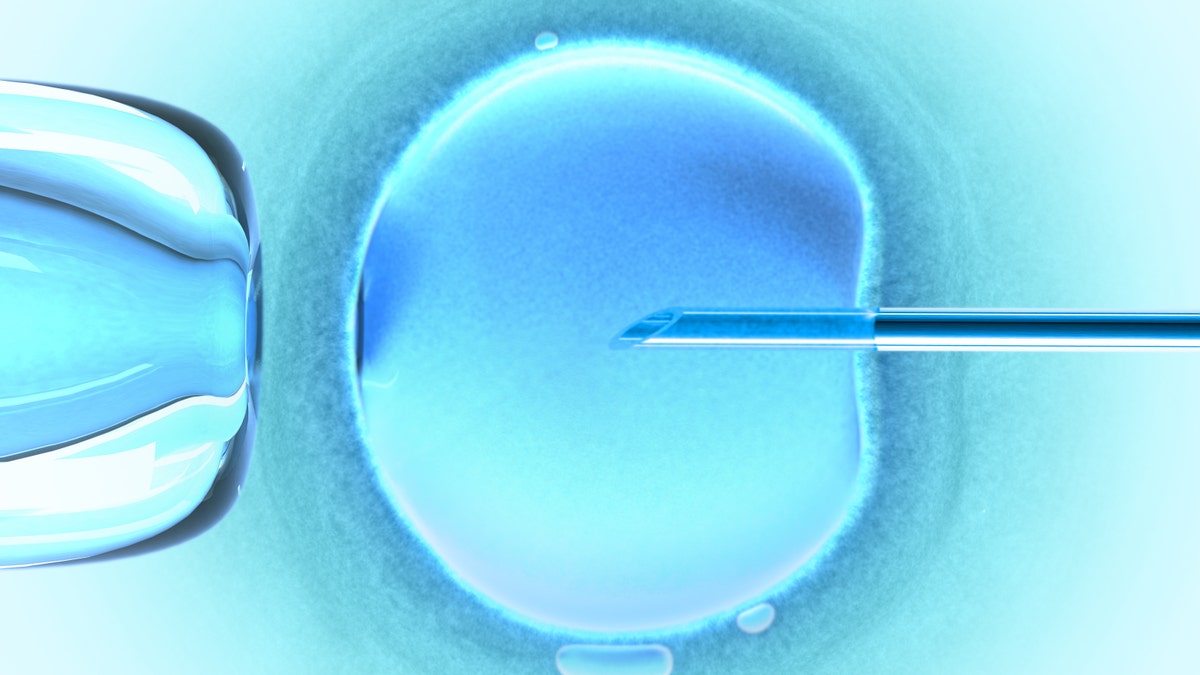
(iStock)
Markie Ricks was 28 when she and her husband, Randall, first flew to Barbados for in vitro fertilization (IVF) treatments. That was in 2013. Four years later, she shares her story.
My husband and I met when I was 20, and we got married after four or five years together. We were engaged for three years before we were married, and we hadn’t been trying to avoid a pregnancy during that time, mostly because I couldn't find a form of birth control that worked well for me and didn't wreak havoc on my hormones. So I had a feeling getting pregnant was going to be an issue once we actively tried to grow our family.
Right after we were married, I started keeping track of my cycles and we tried to time our intercourse with the times I was ovulating. We took herbal fertility remedies, and we tried special diets. After a year, when I still wasn't pregnant, we decided to see a doctor.
6 SIGNS YOU MIGHT HAVE THE SUMMER BLUES
We tried some medications, and did six cycles of intrauterine insemination. But nothing worked. It wasn’t like I was getting pregnant and losing it; I was just not getting pregnant. So our doctors said: “We could do $20,000 worth of tests, because this isn’t covered by insurance. But regardless of what we find, the end game for all potential issues is IVF. So you can do the tests and figure out what’s wrong, or you can jump to the end game and do IVF.”
This was a tough pill to swallow. We wrapped our heads around IVF and started doing research, making consultation appointments with places locally. We’re in Denver, and there are all these renowned fertility clinics here; we were really excited to know we had such good doctors to choose from. But then we went to all our appointments, and were just so disappointed with the doctors and programs and prices. The cost was astronomical! The base price was like $30,000, and that didn’t include drugs or work-ups, which in the U.S. would be many thousands more.
And just the tableside manner of the nurses and doctors we met with was awful. I remember meeting with one doctor, and he basically handed us a price sheet the second we sat down. He then went through the options for treatment, and there was such a push to "upgrade" the treatments and tack on tens of thousands of dollars to our bill. Had the doctor explained why he thought these would optimize our chances, or why our health records indicated that these would be beneficial treatments, it would have made more sense and we may have been more willing to explore these options. But our history was barely discussed. He acted like we were uneducated and completely naïve, and it was both insulting and frustrating. We felt as though these doctors were running more of a business than a medical facility, and to them, we were just a number on a chart. For such an important procedure, and considering it was all out of pocket, we wanted to have a lot of faith in the people providing care for us. And I didn’t.
Randall and I thought there had to be somewhere better and hopefully more affordable, so we did research on international options. This was back in 2013, and there was like zero information out there: no stats or personal accounts. But we just said, screw it, let’s make online or phone consultations with overseas doctors and find out the programs and costs and protocols.
So we had a couple phone consultations, and one of them was a conversation with Dr. Juliet Skinner at Barbados Fertility Center. I was blown away by her. She had obviously pored over my file, and she spent over an hour on the phone with us just laying everything out. She went through my tests and broke them down a bit. For example, she had looked at my ultrasounds and blood work and said that there were no signs of polycystic ovarian syndrome. She said my immune system looked great, my ovulation was regular, my egg count was great, and my husband’s sperm had no issues. I felt very confident she knew what was going on with us, and then she went through, in detail, what she thought was best the option for us.
She recommended IVF with intercytoplasmic sperm injection (ICSI), as she explained that some women’s eggs have a little harder of a shell, and the sperm has trouble actually penetrating them. She recommended a blood thinner to assist with embryo implantation and a steroid to keep my body from "attacking" the embryo. Then she explained exactly what my protocol would be, including all of the drugs I would be taking and why. Not only did I love her, she just seemed so knowledgeable and compassionate. This was not something we’d found anywhere else.
Also, we couldn’t beat the price. It was a fraction of what we’d pay here in the U.S. The price of IVF in Barbados was $5,750, and the drugs were an additional $3,000 in total, so also a fraction of the U.S. cost.
We sat on the information from Dr. Skinner for a couple days, just trying to let it sink in and to think everything through. It felt a little crazy to leave the U.S. for such an important procedure. But we were so frustrated, and this was a beacon of light. It all seemed so positive, so eventually we went for it and booked our trip to Barbados.
It took about six months after we talked to Dr. Skinner to coordinate everything. When we finally went to meet her, in May of 2014, we’d been married five years, and together for almost 10. We were going to a country we'd never been to, and it all felt super scary, but we were so ready for this. Within a day we fell in love with Barbados: We loved the people, it was so beautiful, and the clinic was the cherry on top. Everyone at the clinic knew our names, and they were just the sweetest and most compassionate people you'd ever meet. I remember saying to my husband that if American healthcare were anything like this, it would be a game-changer.
We were in Barbados for two weeks. The day after we got there, we went in for a scan to check my endometrial lining, because I was taking all these drugs to thicken it and make it do what it's supposed to do for IVF. Based on that scan, they adjusted my meds. The drug that they adjust is to control the growth of your follicles. Each follicle holds one egg, and each month, an ovulating female should release one egg. In this scenario, they want as many eggs as possible.
We did a second scan two or three days later. Once the follicles reach a certain size, they prescribe a "trigger shot," which tells your body to immediately release the eggs. The shot has to be taken exactly 12 hours before retrieval. Then all of the eggs are collected the following day through a needle inserted vaginally. The procedure isn’t painful, but there is some uncomfortable recovery as your ovaries have so many more follicles than normal. We scheduled the egg retrieval, and for that I was put under general anesthesia. So they went in and took all my little eggs out. There was no pain, and it was very low-key. Dr. Skinner didn’t do my scans, but she did my retrieval. I'd seen her and met with her, and she was very much a part of everything.
After retrieval, it’s a waiting game, which was both terrifying and exciting. Quite literally, all of our eggs were in one basket! This was our big shot, and we were well aware that if it didn’t work, we’d be devastated, both emotionally and financially. On the flip side, this was the closest we’d ever been to being pregnant, and we were proud of ourselves for taking the leap and just leaning on each other, reminding one another to trust the process.
The next day the clinic called to tell me how many fertilized eggs I had. Twelve were fertilized out of 21 eggs. (That was good. Some people only have one or two fertilized eggs.) So on Day 1, I had 12. Then by Day 3, the nurses called and said we had seven, but they’re "a strong seven." They said they’d do a Day-5 transfer, which is when they implant the fertilized eggs. We were ecstatic! You can do a three-day transfer if the eggs are looking weak, but you want to wait until Day 5. By Day 5, we had five very strong embryos left. The clinic took the top two and transferred them, which left us with three to freeze.
We left two days after the transfer. The clinic does not prescribe any bed rest, and our doctors said that we could fly home immediately after the transfer. When we got home we did the math. For IVF and all the medications, a beach-front suite for two weeks, every meal . . . it all came out to $15,003. Literally half the base cost of what we’d get back home in Denver.
The people at the Barbados clinic told me to wait two weeks to take a pregnancy test. But I couldn’t wait, so after a week I took one and saw a super faint line. I almost thought I was hallucinating. We saw a doctor and found out we were definitely pregnant. And it was a perfect pregnancy, no issue at all. We had our daughter, Remington Rose—we call her Remi—nine months later in February 2015. Easy labor, perfect delivery. Holding her was totally surreal. It made all of the struggles to get to that point worth it, a million times over.
I remember the reactions were mixed when we first told people what we were doing. We weren’t super open with people about our struggles to conceive, but people were excited about our decision to try IVF and wanted to see what would happen. A few were like, "Wait, where are you going? And why would you leave America? Because we’re the best health system." After it all worked out for the best, though, everyone understood.
WHAT IS 'LEAKY GUT' -- AND HOW DO YOU KNOW IF YOU HAVE IT?
To this day, we have no idea what issue was preventing me from getting pregnant. Thankfully, technology exists that we could circumvent it and start a family. We went back to the clinic in 2016, and because we had eggs left, the cost was only $3,000 per visit. It took two trips, but I’m now five-months pregnant with our second child.
My husband and I still look at each other and say, “Can you even believe we are parents?” With a 2-year-old and a baby due in November, we are still in awe that it worked. We are thankful every day that we beat infertility, and even though there were hardships, I feel as though our journey through it all is now part of our story that I wouldn’t ever change.
This article first appeared on Prevention.
