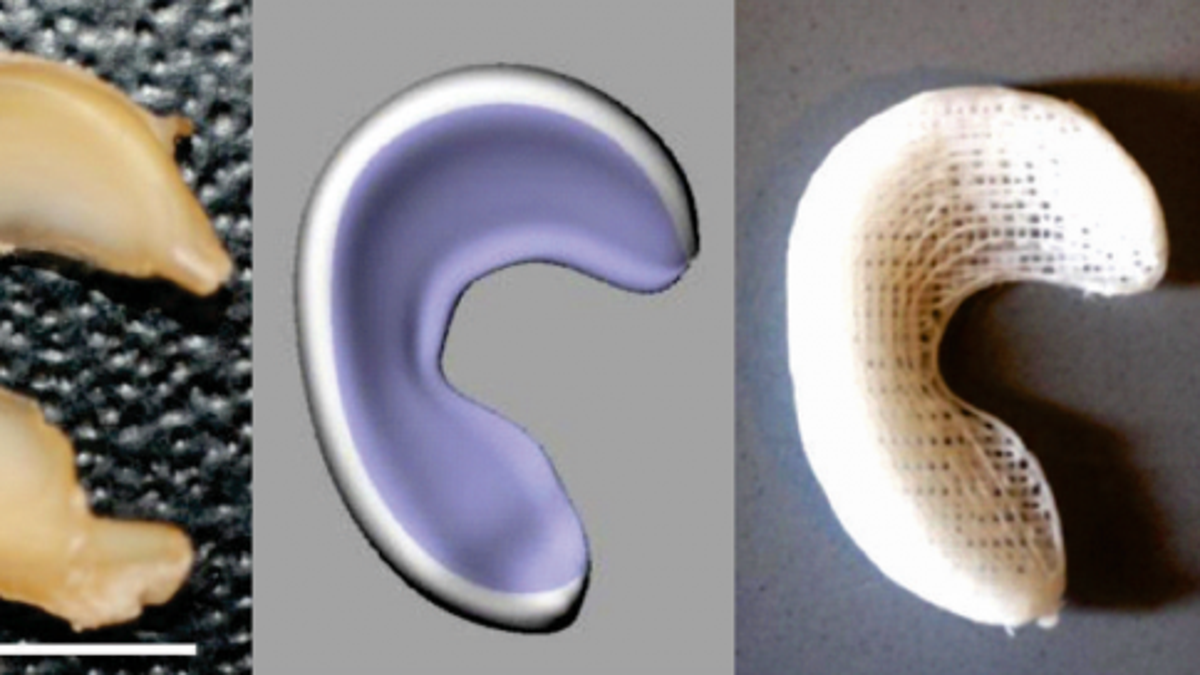
Left to right: Sheep meniscus; 3-D model of meniscus obtained from laser scanning; 3-D printed anatomically correct meniscus scaffold. (Lab of Dr. Jeremy Mao)
3D-printed prosthetic body parts certainly aren’t anything new at this point, but a team of medical researchers at Columbia University Medical Center has just taken the idea to a whole new level. Instead of replacing a damaged body part with an artificial insert, they’ve cooked up a way to use 3D printing in conjunction with stem cells to encourage your body to regrow the damaged part on its own.
Detailed in a recently published study in the online edition of Science Translational Medicine, the researchers have basically devised a way to replace the knee’s protective lining, called the meniscus, using a custom 3D-printed scaffold infused with human growth proteins that prompt the body to regenerate the lining by itself. Over time, the scaffold will deteriorate as the meniscus tissue begins to grow back, presumably leaving the patient with a fully formed, non-artificial joint when it’s all said and done.
The therapy hasn’t been used on humans quite yet but has been successfully tested in sheep (whose knees closely resembles those found in humans) and could provide the first effective and long-lasting repair for damaged menisci, which occur in millions of Americans each year and can lead to debilitating arthritis.
Related: Osteoid is a 3D-printed cast that uses ultrasound to heal your bones 40% faster
“At present, there’s little that orthopedists can do to regenerate a torn knee meniscus,” said study leader Dr. Jeremy Mao. “Some small tears can be sewn back in place, but larger tears have to be surgically removed. While removal helps reduce pain and swelling, it leaves the knee without the natural shock absorber between the femur and tibia, which greatly increases the risk of arthritis.”
Here’s a quick rundown of how the procedure works.
First, doctors conduct a number of MRI scans of the patient’s intact meniscus in the undamaged knee. These scans are used to create an extremely precise 3D model of the meniscus’s shape, which is then sent to a 3D printer. The scaffold is printed out of a special biodegradable polymer called polycaprolactone — the same material that dissolving sutures are made from.
Once printed, the scaffold is infused with two recombinant human proteins: connective tissue growth factor (CTGF) and transforming growth factor β3 (TGFβ3) before being surgically implanted into the damaged knee. Dr. Mao’s team found that sequential delivery of these two proteins attracts existing stem cells from the body and encourages them to form meniscal tissue.
In the trials conducted on sheep, the menisci typically regenerated in about four to six weeks. After three months, treated animals were walking normally. In a postmortem analysis, the researchers found that the regenerated meniscus in the treatment group had structural and mechanical properties very similar to those of natural meniscus. They are now conducting studies to determine whether the regenerated tissue is long-lasting.
If all goes well, trials of this groundbreaking new procedure could begin in humans in 2015.








































