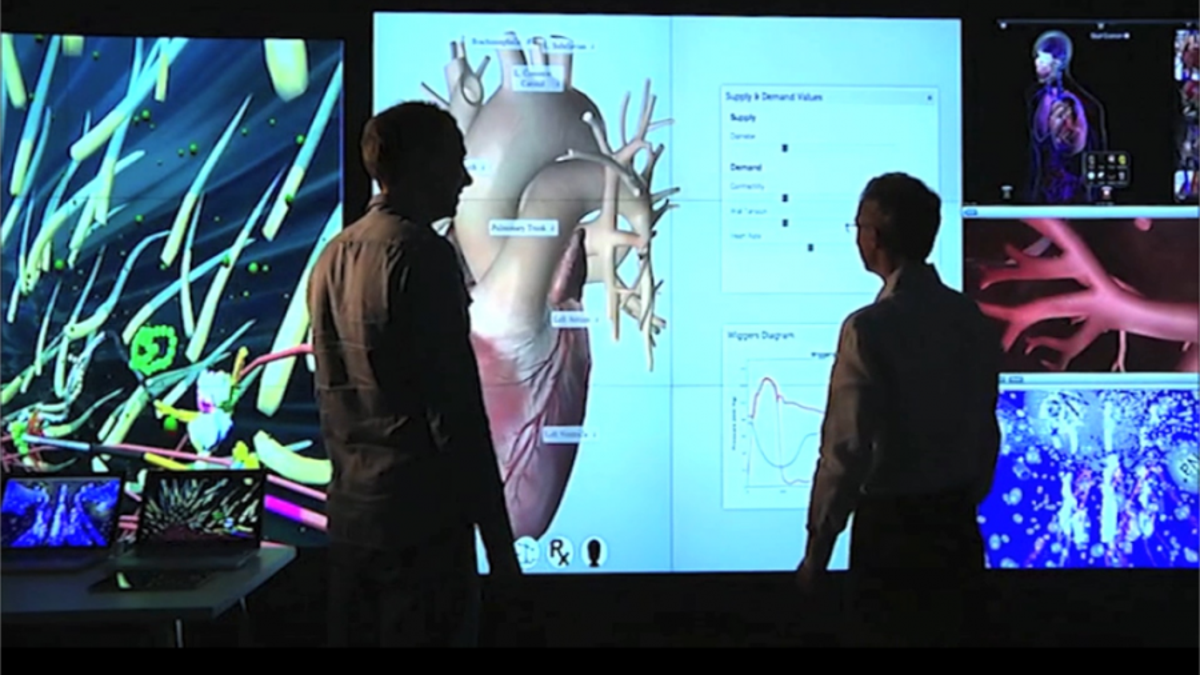
Dr. Christian Jacob with Ph.D. student Timothy Davison working with LINDSAY Virtual Human applications on a display wall in the Visualization Studio at the Digital Library, University of Calgary. (University of Calgary)
We are on the verge of another revolution in health care: deeply personalized medicine. It’s the next computerized step in tailoring medical treatments and medical drugs to your specific body, your very unique anatomy, the specific ways your body works and doesn’t, and your path to live your life and keep healthy.
But we may soon run into problems of ethics and personal privacy that could make the recent furor over Facebook and data mining look small by comparison.
Personalized health and wellness comes from the intersection of improved body-worn sensors, data science, computational physiology, individually customized health assistance and — if necessary — highly targeted medical treatment, all coming together at once.
This dramatic health revolution is enabled by the vastly reduced cost of reading and analyzing our genomes, and of huge, cheap quantities of computer power that allow us to make more precise predictions about our future health from our genetic setup.
As a computer scientist with an interest in complex biological systems — such as the human body — I have been working for some time toward this future alongside medical researchers, physicians, and health practitioners. At the University of Calgary, Canada, we have created the LINDSAY Virtual Human, one of the most advanced interactive medical models in the world, to move the process forward.
But social and ethical complications will also set in. What if our health and life insurers demand access to these intimate personas, with all of their projections, as a condition of writing policies?
LINDSAY is a 3-D interactive computer model originally intended to form the basis for a medical curriculum: the computer model becomes the entry point to understanding human physiology. Human anatomy and physiology is explored through “immersive story telling” enabled by gaming environments combined with virtual and augmented reality. LINDSAY lets us “walk” through the human body, even through a human cell, and gain access to previously unseen biological processes.
The next step is a big one. Can we use LINDSAY to hold, visualize and explain all of our personal medical and health history? Can it include all the processes of each of our individual bodies, to better understand what keeps us alive and healthy? Can we use this to create highly accurate scenarios of our own health into the future?
We all experience a small part of this radical notion now, through the proliferation of health-monitoring apps on our cell phones and other personal devices. My Apple watch takes small samples of data as I live through my busy day. It counts my steps, keeps track of how often I stand, how long I sit, when I should relax and take a breath. And at the end of each day I get a summary, sometimes accompanied with encouragement to do more or just keep at it.
These are very simple reference points for how I am doing with my health. More dramatically, derived from different sensor data, it is already possible to detect early warning signs of, say, irregular heartbeat, and suggest corrective action.
Imagine a computer-driven physiology database so large and detailed that you can build a virtual replica of yourself. Based on input from body sensors, your nutrition plan, your medical history, etc., your “health avatar” could then be used to predict accurately what your body physiology will most likely look like a year from now, or ten years into the future. And we could see the medical conditions that would result.
To make that possible, we rely heavily on massive amounts of personal data. We share it with analytics engines that make predictions and come up with recommendations based on overall trends of your “data cohort,” a significant population as similar to yourself as possible. Then we feed this information into highly sophisticated personal computational physiology simulations to get your unique health projection.
Personal health forecasts will be a lot more intrusive. How far are you willing to go to share your data to accomplish that?
Data from sensors + analytics + computational physiology engines could take much guessing out of your health treatment. For example, in fine-tuning drugs that stabilize medical conditions. Why can’t we try the new drug on your virtual body first?
Imagine the power of natural evolution, but on an immensely faster scale, going through, evaluating, discarding, modifying, and eventually finding the exact personalized drug composition for you. Guessing is over! And you did not have to be part of a lengthy, controlled drug experiment.
The more your virtual body simulation knows about you, the more “smart design” methods, driven by augmented intelligence, can be applied.
But here comes the tricky part. Your personal data alone is likely not enough to give the right recommendations. It needs to be assessed in the context of other people—your “data cohort.” These could be your friends, as you tend to share activities with them. But it could be others with whom you have certain aspects of your life in common: similar jobs, areas with comparable environmental conditions; a certain kind of life style (you tend to go for walks, or try to eat organic food).
Your compiled data will place you in some category. From it, one can derive common patterns, which indicate trends, just like the weather forecast. Or like Tesla’s network of soon-to-be-driverless cars. They gather and share data about road conditions, dangerous intersections, driving patterns etc. and feed the information back into the car fleet and through over-the-air software updates.
Except, personal health forecasts will be a lot more intrusive. How far are you willing to go to share your data to accomplish that?
First steps are already being taken in this direction by bringing patient medical records into personal health apps, as Apple recently announced. This gives us as health care consumers greater control over our own medical data. And we can decide how much — if any — of this data we want to share, for example, with researchers to help find cures for diseases more effectively and faster.
Conceivably, we could even be able to automate our body repair. In the Internet of Things we are creating an industrial nervous system. Through sensors that share their data across extended networks, each component can predict with high accuracy when it’s going to fail — even before it’s actually failing — and order its replacement.
Can we see something similar for your personal health assistant? It may be able to tell you when your knees are going to be worn out — derived from your jogging habits. Can it tell you even before your own body lets you know, and well before your knees start to hurt?
These augmented intelligent systems, which are just starting to emerge around us, should soon give us amazing tools to help us live better, healthier and longer lives.
But social and ethical complications will also set in. What if our health and life insurers demand access to these intimate personas, with all of their projections, as a condition of writing policies? What if our banks make similar demands before issuing mortgages? What can hackers do to the algorithms involved?
Many of these questions are not going to have easy answers — especially the ones we have not thought of yet.
But the time to start thinking about them is now.








































