
FILE -- (AP)
The current opioid crisis in the United States is one issue that unites Americans across the political spectrum.
On July 22, the bipartisan Comprehensive Addiction and Recovery Act of 2016 (CARA) was enacted. The law authorizes the federal government to strengthen opioid addiction prevention, treatment and recovery and expand access to the opioid overdose-reversal drug naloxone.
The Washington Post reported on July 26 that the opioid abuse epidemic, which involves abuse of prescription opioid pain relievers and heroin use, was addressed at both the Democratic and Republican national conventions.
Unlike earlier heroin epidemics, which disproportionately affected inner-city minorities, the current heroin epidemic disproportionately affects white, middle-class people in non-urban settings, as shown in research published in JAMA Psychiatry. Among the groups most affected are the privately insured:
According to the Centers for Disease Control and Prevention (CDC), heroin use increased 63 percent from 2002-2004 to 2011-2013 among people with private or other health insurance, excluding Medicaid.
As stewards of the nation’s largest database of privately billed health care claims (over 20 billion records), my organization FAIR Health, has a unique vantage point from which to study the impact of the opioid crisis on the privately insured.
We reported our research in a new white paper, The Opioid Crisis among the Privately Insured: The Opioid Abuse Epidemic as Documented in Private Claims Data, and in the infographic below.
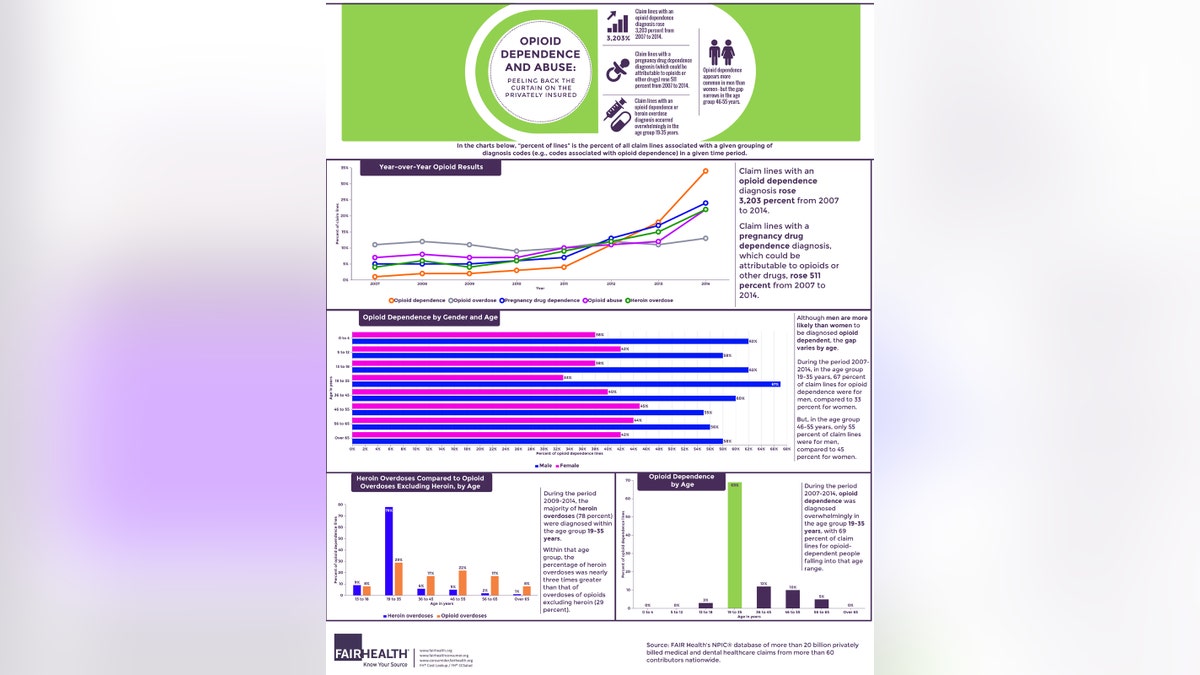
According to FAIR Health data, claim lines with an opioid dependence diagnosis rose 3,203 percent from 2007 to 2014. Claim lines with a pregnancy drug dependence diagnosis, which could be attributable to opioids or other drugs, rose 511 percent. In a number of states across the country, opioid dependence was diagnosed more frequently than all other substance abuse and dependence diagnoses combined.
Among overdoses from various opioid types, the greatest increase has been in heroin overdoses, which grew 510 percent from 2009 to 2014. Moreover, heroin overdoses during that period increased more quickly than overdoses from prescription opioid pain relievers and street drug opioids excluding heroin.
People aged 19 to 35 years show a higher propensity for opioid dependence and heroin overdose diagnoses than other age groups, according to FAIR Health data.
That age range accounted for 69 percent of claim lines for opioid dependence during the period 2007 to 2014, and 78 percent of claim lines for heroin overdoses during the period 2009 to 2014.
In the period 2007-2014, that age group also represented 50 percent of claim lines for opioid abuse, a less severe clinical diagnosis than opioid dependence.
There are a number of signs of women’s increasing involvement in the opioid crisis. Although the CDC reports that men are more likely than women to die from prescription opioid overdose, FAIR Health data for the period 2007-2014 indicate that women were more likely than men to be diagnosed with opioid overdose (53 percent versus 47 percent, respectively). Men in all age groups are more likely than women to be diagnosed opioid dependent, but the gender gap varies by age, and appears particularly narrow in the age group 46-55 years.
For example, in the period 2007-2014, 55 percent of claims for opioid dependence in that age group were for men, compared to 45 percent for women. Opioid abuse also was diagnosed more often in women than men in 2014. This inversion of the usual gender pattern of opioid-related diagnoses, which may reflect more opioid abuse or differences in the way men and women are evaluated for this condition, merits further study.
We hope that FAIR Health’s findings will contribute to the important national conversation about the opioid crisis.








































