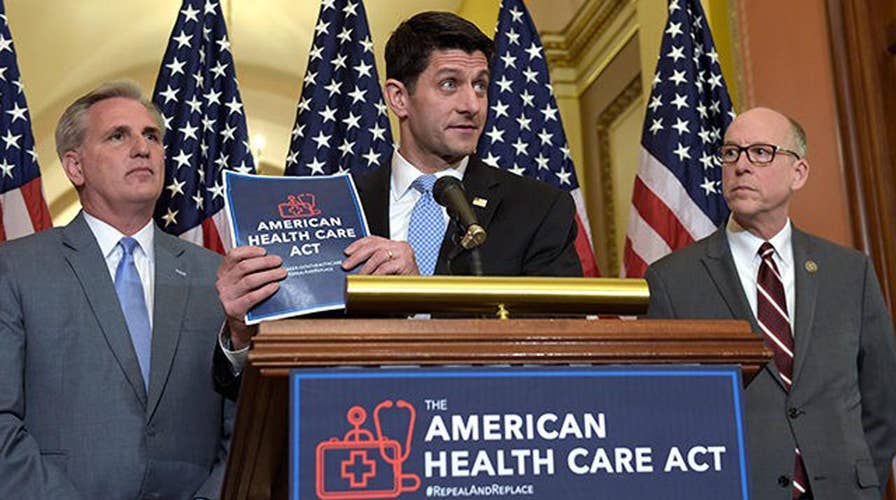
Sources say WH aiming for health reform vote on Wednesday
President Trump wants a vote because the repeal and replace of ObamaCare was a central campaign promise and it frees up more money for tax reform; John Roberts has the roundup for 'Special Report'
While there is still some uncertainty over the exact timeline and a comprehensive alternative plan, it certainly appears that the Affordable Care Act – or at least significant components of it – will be greatly altered in the near future. The passage of the Republican-backed health care bill in the House on Thursday brings us one step closer to change.
For health care providers across the country, the current ambiguity is maddening.
After six years of scrambling to adapt to many changes brought on by the ACA, many are now wondering how, and how quickly, they will need to change (again) in 2017.
But lost in the controversy over when, or whether, the ACA will be fully repealed is an arguably more powerful force in health care: the rapid erosion of the fee-for-service system. With its massive volume incentives, disjointed care infrastructure, and huge costs, fee-for-service medicine has been dying for years, and is being replaced by risk-based models, where providers own a financial stake in the quality of care they deliver to patients.
Thus, while federal policy is on the cusp of major change, one thing is set in stone: health care providers must continue to build an infrastructure that supports higher-quality, lower-cost health care delivery.
The pillars of this new infrastructure are commonly understood in all segments of the industry: technology (both patient-facing and internal), care management resources, a right-sized inpatient to outpatient ratio, and patient-centric models of care. But the most important infrastructure is the human capital that underlies everything. So an investment in people is perhaps the safest bet health systems can make right now.
To start, this advanced infrastructure requires new roles that do not yet exist in many institutions, from care managers, patient navigators, and nutritionists to call center operators, community health workers, and more. According to the Bureau of Labor Statistics, the prevalence of personal care aides alone is expected to increase by almost 50 percent by 2022. Similar increases will be seen for physician assistants, physical therapists, and nurses.
At the same time, many inpatient jobs could disappear as outpatient and ambulatory departments expand. Some job categories will simply need many fewer workers overall — janitors, food service, housekeeping, as examples — and health systems should look to retrain these individuals into the roles of the evolving system.
Some job categories will need fewer workers on the inpatient side, but many more in new areas like ambulatory and urgent care. Demand for nurses, for example, is expected to grow only marginally on the inpatient side over the next ten years, but grow rapidly for outpatient care.
Workers will also need to be trained in health care methods that support prevention and reduce hospitalization. For example, home health aides will need to use tablets to report on real-time patient conditions directly to primary care doctors.
Physicians will need to be fluent in telemedicine models to care for patients in their homes.
Nurses will need to be trained in care coordination tools to improve continuity of care as patients move through health care settings.
If health systems are serious about reducing cost and improving outcomes, the workforce must be trained to use technology that shares data, manages care, and empowers patients outside the walls of a hospital or a doctor’s office.
Health systems can also use data to better understand their workforce. An internal dashboard of cost and quality can show hospital leadership which physicians offer the most value in their care. This could both initiate corrective action and help steer patients towards the best care.
Data tools can also help predict which workers will succeed in the jobs of the future, based on their previous work history and new hospital environments.
Some might be a great fit for some roles, and not very good for others; perhaps a former janitor will make an excellent care manager with a robust training program. Predictive tools can help make this determination
Building a trained workforce to match the ongoing shift in care delivery takes time, resources, labor-management partnership, and long-term commitment.
Even amidst a deep political fog, much of the work ahead remains quite clear. Population-based health care is the way of the future, and its demands require long-term change and commitment that cannot be swayed by the political winds.