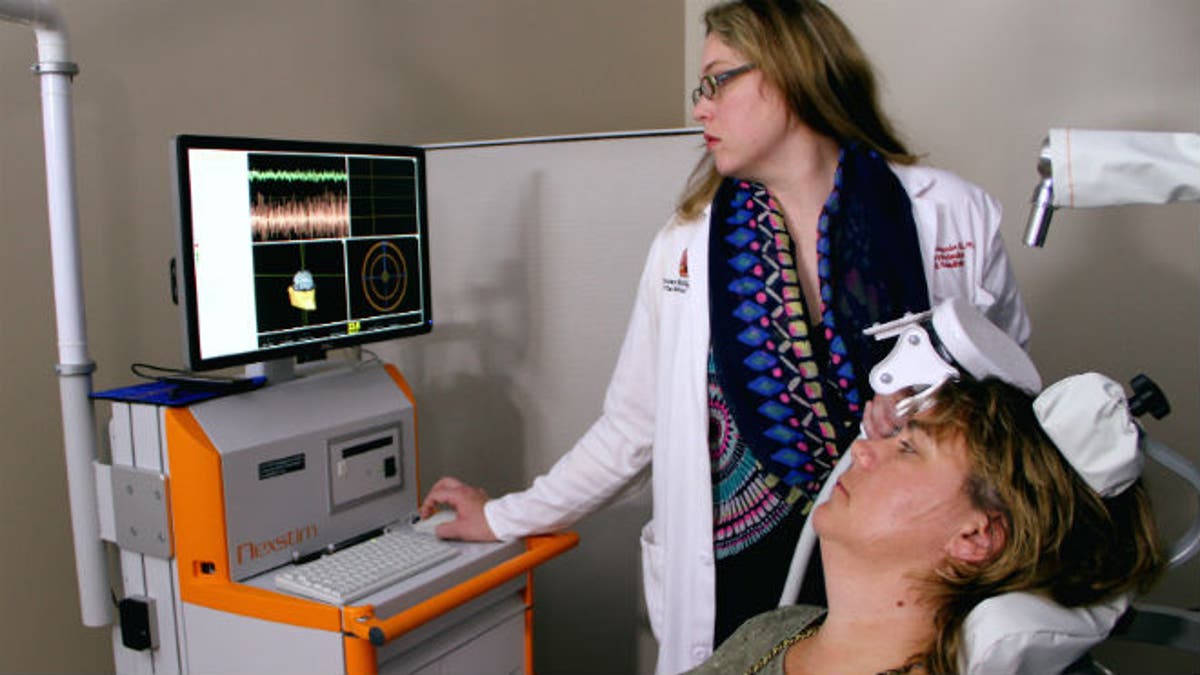
Dr. Marcie Bockbrader adjusts an external brain stimulator on stroke survivor Debbie Hall at The Ohio State University Wexner Medical Center.
In an ongoing multi-center clinical trial, researchers are studying whether transcranial magnetic stimulation and occupational therapy can improve recovery for stroke patients.
For the study, patients are treated with transcranial magnetic stimulation, which stimulates a specific part of the brain using the Transcranial Magnetic Stimulator (TMS) by Nexstim (the technology developer who is funding the study), to help improve activity in the side of the body injured by stroke. The study currently has about 60 participants in 12 centers, but researchers are aiming to recruit 200 patients.
During a stroke, the blood vessel that carries oxygen and nutrients to the brain is blocked by a clot, called an ischemic stroke, or ruptures, known as a hemorrhagic stroke, depriving part of the brain from blood and oxygen. This leads to brain cell death and lasting deficits, which can include changes in speech, as well as vision and memory problems.
A patient may also lose feeling and movement in one side of their body due to decreased activity and function in the side of the brain injured by stroke.
The decrease in activity is similar to “a negative feedback loop, such that the less activity that those neurons have, the harder it is for them to recover function— and the greater the activity on the healthier side of the brain,” principal investigator Dr. Marcie Bockbrader, assistant professor of physical medicine and rehabilitation at The Ohio State University Wexner Medical Center, told FoxNews.com.
“This imbalance actually prevents— to some extent and to some people— the recovery of function on the injured side,” she said.
One therapy to address this imbalance is to physically constrain the healthy side of the body to allow the injured side of the brain and body to express itself.
While not all stroke patients experience this imbalance, a large proportion does. The study authors intend to demonstrate that delivering inhibitory stimulation to the healthy side of the brain combined with occupational therapy sessions, prompts increased activity on the injured side of the brain— and results in better function on the side of the body weakened by stroke.
Previous studies have shown brain stimulation alone does not provide enough benefit, so combining the process with therapy is key, Bockbrader said.
To participate, patients must have had a stroke within three to 12 months of enrollment, and have some one-sided upper-limb deficits but still have some upper-limb function in order to do the occupational therapy exercises.
Bockbrader noted that researchers have been selective and, to avoid confounding variables, can’t accept people with severe deficits, multiple sclerosis and spinal fusion. Patients must be close enough to their study center to go in three times a week to receive their therapies over the six-week course.
Because most health insurance covers only three months’ worth of therapy, researchers have found success recruiting at physical and occupational therapy sites. The study provides free therapy for six weeks for all participants.
“Everybody benefits, whether or not there’s added benefit from brain stimulation. That’s a bonus,” Bockbrader said.
For the double-blind, randomized trial, participants undergo six weeks of the combination of brain stimulation and occupational therapy. Half of the group receives sham stimulation and the other receives active stimulation. Once the data is collected across all the sites, researchers will reveal participants’ information and evaluate their functional ability to use the arm on their weaker side. Bockbrader expects the study to continue for another year or two as they gather data.
“What this would tell us is if the brain stimulation is working more than just therapy alone,” Bockbrader said, “making the neural ‘pop’ that is needed to change and increase their activity on the injured side of the brain … by suppressing the healthy side of the brain.”
The TMS treatment
Once participants are accepted into the study, an MRI scan of the brain is taken to understand the motor areas affected so researchers can target the magnetic pulse. The pulse is strong enough to illicit a twitch in the person’s healthy arm, so researchers know they’re aiming for the part of the healthy side of the brain assisting with motor function of the arm or hand.
“We can get something like 2 millimeter accuracy when we’re delivering 900 stimulation pulses over the course of 15 minutes, so it’s a 3D targeting within the brain based on the individual patient’s motor area for their hand,” Bockbrader said. There is also an orientation rotational component so researchers know the magnet is oriented in a way that maximally stimulates the correct neurons.
Participants sit in a comfortable reclining chair during the treatment. Once their stimulation intensity is determined, the Nexstim device is placed next to the head against the patient’s scalp, and delivers rapid magnetic pulses that go directly to their motorcortex to inhibit activity on the healthy side. A tracker on the patient’s forehead and an infrared sensing system tells the device’s navigation system if the pulses are on target, or if the Nexstim coil needs to be moved. After 15 minutes, the patient is done and goes on to the occupational therapy session.
The stimulation threshold is dependent on the state of the brain at the time, which means that each time a patient comes in for his appointment, it is recalibrated to get the same amount of motor response each time. Eventually, researchers hope to be able to prescribe individual patients a specific strength of pulse, for a specific duration of time in a particular brain area.
Researchers re-examine patients six months after treatment to see whether the benefits are sustained.
TMS beyond stroke rehabilitation
Researchers hope that future phase III research will show enough evidence that the brain stimulation therapy can be adopted as a way to help people who have persistent deficiencies after a stroke.
The therapy can also potentially be pointed at any part of the brain that needs to be modulated after a stroke. Noninvasive brain stimulation may also be useful for non-stroke related issues, such as fatigue, attention, and mood, Bockbrader said.
“I also see patients with traumatic brain injury and the protocols are similar across brain injury types…. So you can apply some of the technology to problems that result from brain injuries of different types,” she said.
One unknown is whether the therapy would work when administered beyond a year after stroke incidence.
“Theoretically it seems possible, but until we test… we just don’t know,” Bockbrader said. “[After a year] the spontaneous recovery period from stroke is essentially over, so if we could reinstitute a state of being more receptive through therapies to drive plasticity, that would improve function and drive recovery.”
Once the treatment is approved by the Food and Drug Administration (FDA), Bockbrader expects it would be marketed immediately in the clinical setting.
“From my point of view as a clinician, that’s what’s important— what we do in terms of man on the street,” she said. “Can they get this to help them get better? We want to make it more widely available.”







































