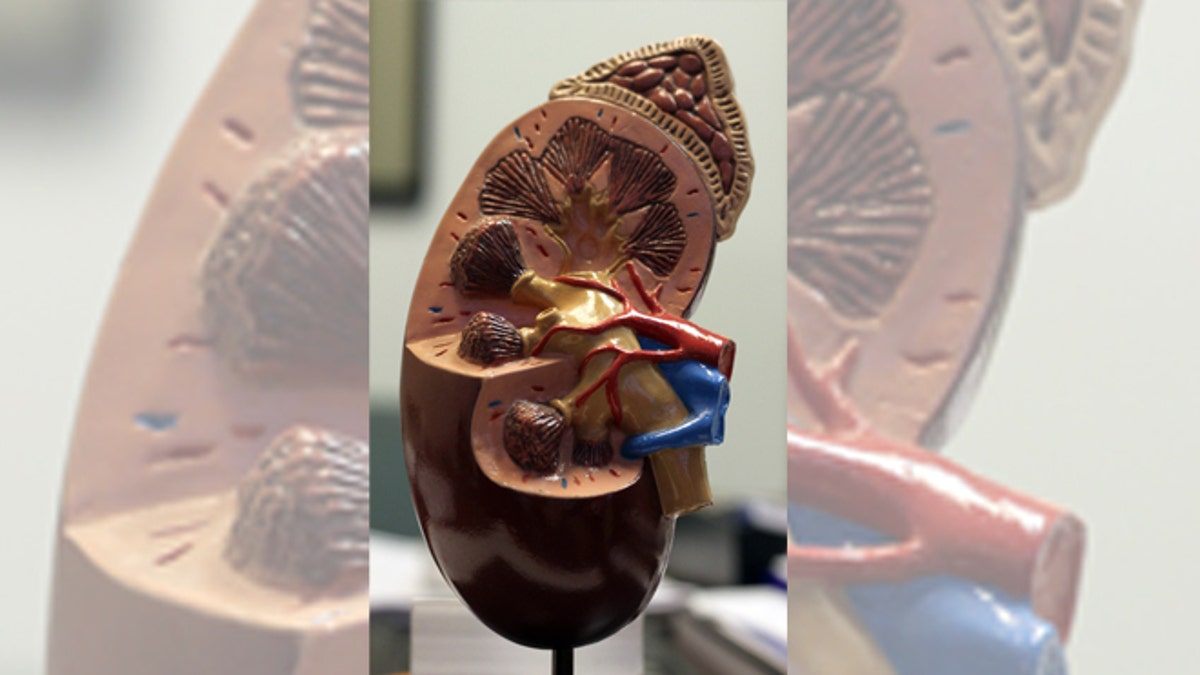
(Courtesy of the National Kidney Foundation)
A new study suggests that kidney failure can be predicted based on measurements taken in adolescence.
The research, published in the National Kidney Foundation’s American Journal of Kidney Diseases found that high blood pressure, being overweight, elevation of a blood marker indicating inflammation, or the presence of protein in the urine of healthy male teens were all independent predictors of end stage renal disease later in life.
“We were surprised by the magnitude of the risk, especially for individuals with unexplained proteinuria in adolescence,” Dr. Per-Ola Sundin, lead study author and physician at Orebro University Hospital in Sweden, said in a news release. “This shows that kidney damage is already occurring in teenagers who won’t develop more noticeable symptoms of kidney disease for many years,” Sundin said.
The study analyzed Swedish male residents in the 1970s who had physical examinations done when they enlisted in the military at around 18 years old. Of that group, 534 men developed end stage renal disease later in life, the researchers said.
The data collected showed a presence of proteinuria in the physical examination was associated with a seven-fold increase of end stage renal disease. Researchers said despite the study’s focus being Swedish males, there was no reason that the findings would not hold true for females and other populations.
Other factors, like being overweight and high blood pressure were also found to increase the risk for the disease.
“These results suggest that there is a screening opportunity at early an age if we want to prevent chronic kidney disease,” Sundin said in the news release. “Particularly, proteinuria without an explanation should be followed up by doctors and patients. Also, it is never too early to tackle issues like unhealthy weight gain and hypertension as it may be much harder to begin a healthy lifestyle in later adulthood.”
According to the National Kidney Foundation, one in three Americans is currently at risk for developing kidney disease.







































