As U.S. health officials scramble to identify a growing list of possible Ebola patient contacts after the diagnoses of two Dallas nurses who contracted the disease while treating Thomas Eric Duncan – many Americans are wondering what the process entails.
The Centers for Disease Control and Prevention (CDC) and Texas health officials are monitoring 48 close contacts of Thomas Eric Duncan, the first patient diagnosed in the U.S. After a nurse, Nina Pham, contracted the virus while caring for Duncan, 77 health care workers went into monitoring. Now, 132 passengers on a Frontier Airlines flight are being contacted after another nurse, Amber Vinson, was diagnosed on Wednesday.
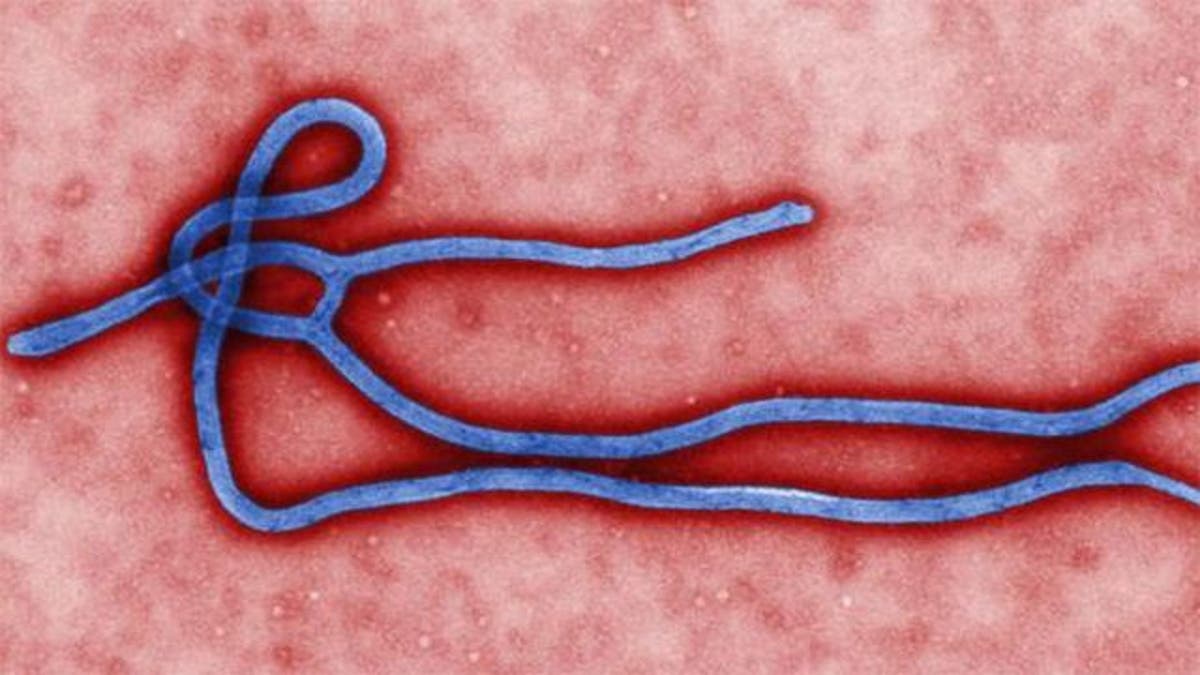
Ebola, which is spread through contact with the bodily fluids of a symptomatic patient, has a transmissible period of 21 days. Under CDC guidelines, everyone who comes in direct contact with a symptomatic Ebola patient are watched for signs of illness during that period. If a contact develops a fever or other Ebola symptoms, such as diarrhea and vomiting, they are isolated, provided care and contact tracing begins for them.
From an epidemiology point of view, Ebola differs from other infectious diseases because the morbidity and mortality rates are higher, so a larger number of contacts are traced.
“They’re likely expanding the list wider than needs to be just to be on the safe side, and that the only way people can acquire it is through the bodily fluid transfer,” Dr. Anthony Harris, professor of epidemiology and public health and University of Maryland School of Medicine and incoming president of the Society for Healthcare Epidemiology of America (SHEA) told FoxNews.com.
“The way contact tracing basically works is it’s almost like a social network—casting the net generally as widely as possible,” he said.
With Ebola, it’s difficult to know exactly when a patient acquired the virus or when they became symptomatic, he noted. However, because the disease spreads only through bodily fluids, the transmission risk is lower than other diseases, such as the common cold or influenza, which are airborne.
“The person on the street is not going to get Ebola, I think that message needs to be clear,” he said.
In the case of the two nurses, while it’s unknown exactly how they were infected, it likely happened because the health care workers were exposed to a large volume of bodily fluids during the first three days of Duncan’s hospital stay, according to the CDC.
“[Duncan] was more infectious in that period due to the amount of bodily fluids,” Harris said.
Pham and Vinson both admitted themselves to the hospital when they were experiencing fever and no other symptoms.
“When the person just had a fever, the potential for transmission is much lower… the bottom line is, we do know [if there is] no contact with bodily fluid, the risk of transmission is zero, that’s clear,” he said.
As for the risk of those who live in the apartment building of or flew with the second nurse, it can't be answered without knowing her symptoms and at what point in time she had them relative to being around the apartment personnel or passengers, Harris said, noting that because the virus is only transmitted by bodily fluid contact the risk should be extremely low.
Mathematical modeling has shown the transmission rate of Ebola in West Africa — meaning the number of people a sick patient is likely to infect — is two, but that doesn’t apply to the U.S. because the infrastructure is different.
“The breakdown in West Africa, unfortunately… is an infrastructure problem — lack of hospital epidemiologists, lack of ability to isolate people, lack of gloves and gowns, lack of education about how to put on and remove them, and then the burial practices,” Harris said, noting that at Emory University Hospital and Nebraska Medical Center, the transmission rate has been zero.
Hospital epidemiologists are infectious disease specialists who are trained to deal with contagions and prevent patients from getting any infection within the hospital. They go through protocols to ensure a patient is isolated quickly, triage patients for low or high probability, practice drills, train in putting on and removing personal protective equipment.
“They’re fully equipped to deal with these types of outbreak situations, this kind of triage … we’ve done it before with MERS-CoV, SARS,” Harris said. “This is what we do on a day-to-day basis.”
Ebola won’t be controlled by a ‘magic cure,’ but by known infectious disease control measures such as wearing proper protective equipment, and using experienced health care workers who know how to put on and take off personal protective equipment safely, he said.
“The general public should not be worried at this point,” Harris said.







































