Rise in coronavirus cases pushing healthcare limits
Chief Medical Officer at MDstaffers Dr. Dan Field joins Trace Gallagher to give insight into the healthcare system amid the coronavirus outbreak.
Get all the latest news on coronavirus and more delivered daily to your inbox. Sign up here.
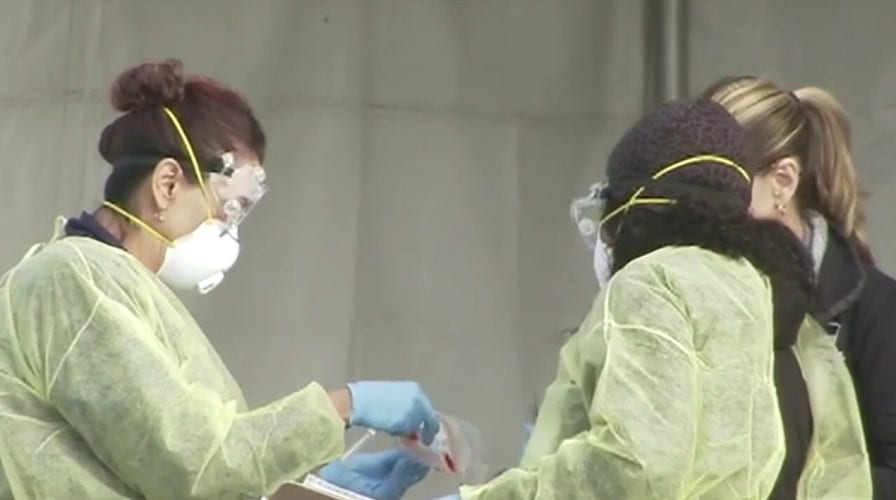
Frontline health care providers around the country are sounding alarm bells about the rationing of protective gear and lack of rapid response COVID-19 testing -- and some are even doing so from quarantine.
Distressed doctors and other health care professionals have been sidelined from the pandemic response because they have suspected cases of coronavirus. They are home with their quarantined spouses and kids, but in a sign of how disjointed the coronavirus response has been, some doctors have no idea if they are actually infected.
NYC HOSPITAL STAFF SEEN WEARING TRASH BAGS FOR PROTECTION, CO-WORKER DIES FROM INFECTION
"It's pretty frustrating that we have celebrities and basketball players getting tested the same day," said Dr. Damian Caraballo, a Tampa emergency room physician who had been quarantined for a week before learning he was negative. "But if you're a doctor or nurse you can't get tested [immediately]. You're waiting six or seven days to find out your results."
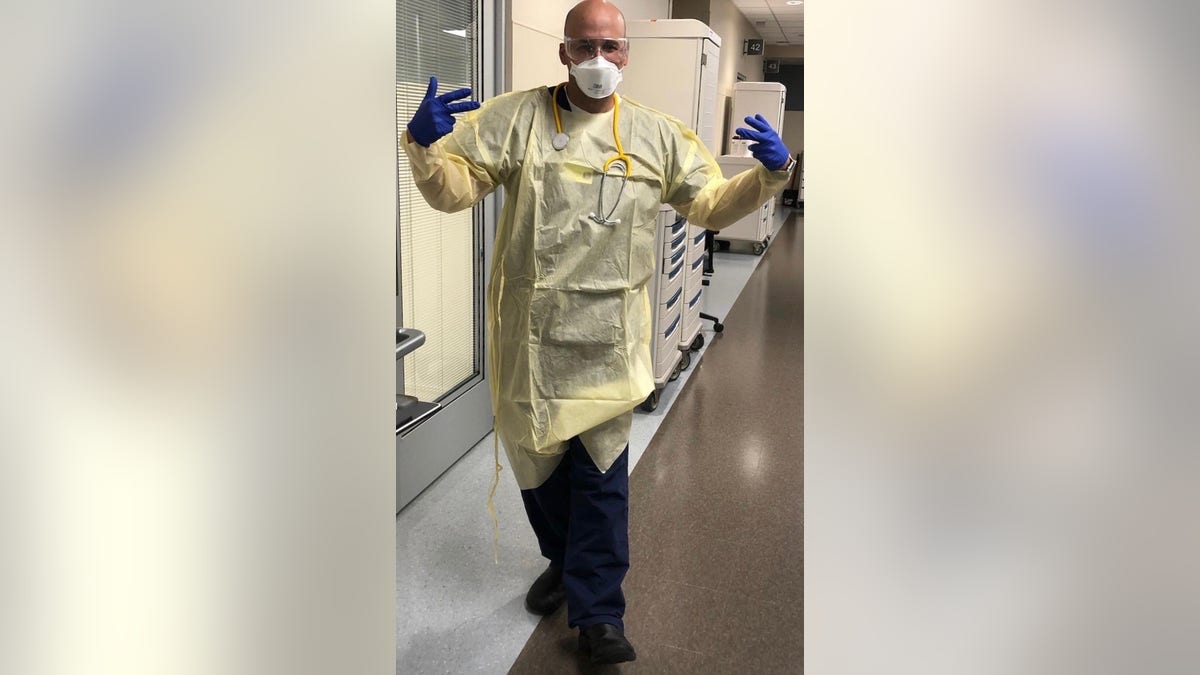
Dr. Damian Caraballo, a Tampa emergency room physician, was quarantined after treating COVID-19 patients. He had to wait 6.5 days for his test results to come back negative.
Full NBA teams have already been tested for the coronavirus. The Brooklyn Nets paid a private company to get the tests and learned four players were positive. Politicians are getting tested and finding swift results. Sen. Mitt Romney, R-Utah, was tested Monday and got his negative results back the next day. Vice President Mike Pence and his wife were tested and seemingly received their negative results within hours.
Meantime, Caraballo, 39, and at least one of his colleagues had been home quarantined and presumed infected from one of the COVID-19 patients he's treated in the emergency room. He's joined with other health care professionals around the nation saying the lack of N95 respirator masks and other protective gear is a dangerous embarrassment that will lead to more doctors out of commission and unable to treat the rapidly spreading virus.
Not only is the dwindling supply of masks, gowns and gloves putting health care workers in peril, but the lack of widespread rapid response testing means doctors don't even know what patients coming into their hospital need to be isolated, the doctors say.
CORONAVIRUS: WHAT YOU NEED TO KNOW
Patients can come into the emergency room without any coronavirus symptoms, for conditions such as a broken ankle, and they aren't in isolation. Doctors aren't necessarily suited up in gear for asymptomatic patients for rationing reasons. But the danger is that patients may still be infected without obvious symptoms and unprotected health care professionals are at grave risk, doctors say.
Dr. Haig Aintablian, president of the American Academy of Emergency Medicine Resident and Student Association, said up to 100 ER residents are in quarantine nationwide and the main two factors are lack of rapid testing and lack of personal protection.
"It’s a complete mess, and our government is not doing enough to fix this issue," Aintablian told Fox News.
NYC'S ELMHURST HOSPITAL AT CORONAVIRUS BREAKING POINT AS 13 PATIENTS DIE IN 24-HOUR SPAN
"I’ve heard from numerous residents nationwide that they are being denied appropriate PPE (personal protective equipment) by administrators, likely due to a huge shortage," he said. "Some residents are being handed one N95 mask to use for weeks at a time. We all know these masks are single-use, and using them multiple times can not only spread viral particles but also prevent their function in protecting our trainees."
Doctors around the country have varying supplies of personal protective equipment. Some say they have enough gear now, but have to ration their masks because they don't know when replenishments are on the way. Doctors want the ability to do on-site testing with results back in under an hour so they can accurately isolate patients and protect themselves.
Dr. Purvi Parikh, an immunologist in Manhattan, works in a clinic treating patients with allergies, asthma and immune deficiencies – a population that’s at a higher risk to contract COVID-19. But her office is out of N-95 masks and gowns and every time they try to place a new order it gets canceled.
She’s had to reuse her N-95 over and over again for the last week. She’s also down to her last box of less protective paper surgical masks. They’ve had to lock up the rest of the surgical mask supplies after a few boxes were stolen.

This is the last box of surgical masks in Dr. Purvi Parikh's Manhattan office. (Contributed photo)
“I've basically just been spraying the outside [of my N95 mask] with Lysol and hoping for the best," Parikh said. "All doctors are sharing tips on how to sterilize something that's not meant to be sterilized.
"These are disposable items you're supposed to be using a different one with every single patient, whereas we're using it for like days on end," added Parikh.
Still, she considers herself lucky.
"People are jealous of me when they hear I have one [N95]. That's how crazy it is," she said.
DO YOU QUALIFY FOR A STIMULUS CHECK IN SENATE’S CORONAVIRUS RESPONSE BILL?
As more health care workers are quarantined or testing positive around the country, doctors said without the proper equipment and tests, more in their ranks will be knocked out.
It's unclear nationwide how many health care workers so far are quarantined or have tested positive.
But the statistics available show a grim picture. In Ohio, about 16 percent of COVID-19 cases are health care workers, Cleveland.com reported Wednesday. And in Italy, France and Spain, more than 30 health care professionals have died of the coronavirus, and thousands of others have had to self-isolate, the New York Times reported Tuesday. In Spain, nearly 14 percent -- or 5,400 people -- of the country's confirmed coronavirus cases are medical professionals.
In the U.S., at least two ER doctors, one in New Jersey and one in Washington state, were infected with coronavirus and were in critical condition, the American College of Emergency Physicians announced March 14.
Then on Tuesday, Kious Kelly, assistant nursing manager at Mount Sinai West in Manhattan, died after contracting the novel coronavirus, the New York Post reported. The lack of protective gear at his hospital was so dire that nurses were wearing trash bags.
Parikh, the Manhattan doctor, said the toll on health care workers is “heartbreaking" and especially tragic when professionals are resorting to office supplies to make masks just to do their jobs.
“It’s very scary because that could be me or anyone of my friends,” Parikh said after learning of Kelly's death.
"If we lose our health care workforce, then who's going to take care of all of the patients?" she said.
Caraballo, whose family of five was quarantined for nearly a week before getting his negative test result, called the lack of protective gear and the lack of knowing who is sick a "perfect storm."
Doctors aren't advised to be fully suited up for asymptomatic patients because of a scarcity of masks and then health care workers can get sick and pass it along to others. With testing taking so long, infected people unknowingly spread the virus "exponentially."
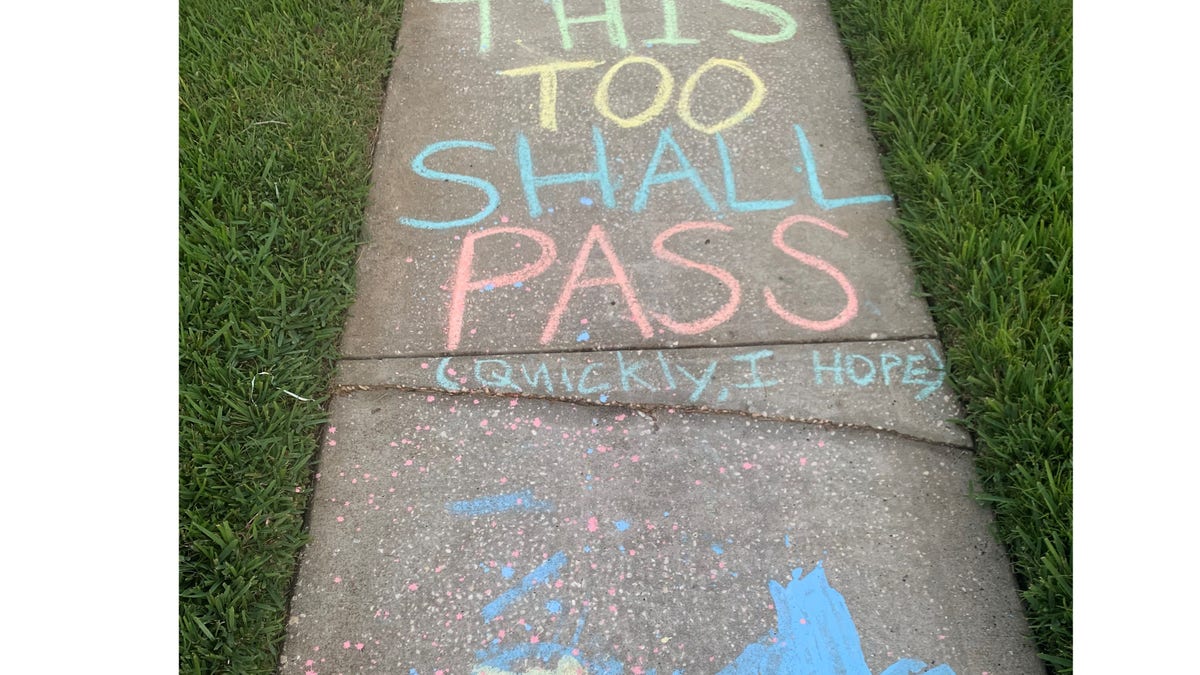
Dr. Damian Caraballo is quarantined in Tampa after treating COVID-19 patients. This is message from kids in his neighborhood. (Contributed photo)
Health care professionals Fox News interviewed for this article made clear their opinions are their own and don't represent the hospitals or institutions that employ them.
But throughout the country, doctors were sending out an SOS message that the lack of armor, leadership and intel going into the war against the pandemic is causing great anxiety for health care workers.
"Everybody is on the edge of their seat. ...Online, it's a powder keg. I mean I've never seen [health care] providers so anxious in my life," Caraballo said.

Dr. Damian Caraballo was quarantined with his wife and kids in Tampa while awaiting his test results. (Contributed photo)
Caraballo's nasal test swab was sent out to California where he had to await the results for 6.5 days. It's been frustrated to see other countries -- like South Korea -- have widespread testing and their doctors wearing what looks like spacesuits to treat patients, he said.
Meanwhile, the Centers for Disease Control and Prevention (CDC) is advising doctors dealing with a shortage of facemasks to use a bandana or scarf to care for COVID-19 patients as a last resort. Health care professionals without masks in contact with a COVID-19 patient are advised to stay away from work for 14 days, setting up a scenario for many more doctors and nurses to be absent from the frontlines.
“The CDC recommendations sound like we’re in a third world country," Caraballo said.
The White House coronavirus task force has been working for weeks on boosting the supplies of protective gear and the availability of tests, but providers on the ground say the relief hasn't come soon enough. The next big issue is a shortage of hospital ventilators when a community is overwhelmed with sick people who need hospitalization.
Congress is on the verge of passing a nearly $2 trillion stimulus package that should also send aid to hospitals, but frontline workers say they can't wait any longer for relief. It passed the Senate unanimously on Wednesday and is set for a vote in the House on Friday morning.
SENATE OKS $2T CORONAVIRUS STIMULUS PACKAGE IN UNANIMOUS VOTE; HOUSE SETS FRIDAY VOTE
The lack of testing, scarcity of personal protective equipment and changing medical guidance have taken a toll on frontline workers, many of whom are dealing with the added stress of children home from school and daycare.
“It's very chaotic and very scary. In a lot of ways, we feel a little bit helpless,” said Dr. Amy Cho, an emergency medicine physician in Minnesota and mother of four children.

Dr. Amy Cho, an emergency medicine physician in Minnesota, called the situation chaotic and scary. (Contributed photo)
Almost three weeks ago, Cho's independent physician practice was moving forward to set up drive-thru testing at one of their urgent care facilities in the Twin Cities area, but the effort had to be quashed for lack of masks for health care workers, she said.
“The situation is really desperate,” Cho said. “We don't have the ability to test. We don't know how prevalent it is in our communities because there's been no surveillance testing. So we don't even have the ability to make an educated guess. We're flying blind and the direction changes over and over again.”
As she and her colleagues treat COVID-19 patients, they are acutely aware they may become sick themselves. Already one doctor Cho works with was out with symptoms but returned after testing negative.
“I’m friends with everybody I work with. I'm worried. Statistically what will happen is people on my teams will die from this and it will happen because they're at work and they're doing their job,” Cho said. “And I'm very terrified of that.”
Some health care employees have panned the CDC guidelines as being based on the scarcity of resources and not based on science. While CDC guidelines recommend protective gear when caring for COVID-19, some professionals have taken matters into their own hands ---- especially since COVID-19 patients can show no symptoms of illness.
"You walk into a hospital, you have no idea who actually has this disease unless every single person has been tested," said Dr. Christian DiPaola, an orthopedic spine surgeon in Massachusetts, who --like many health care workers in recent days--describes the hospital as a "battle zone" because it's the most likely place healthcare professionals would come in contact with a COVID-19 patient.
So DiPaola decided to wear his surgical gear all times in the hospital -- an operating room hood, mask, scrubs, protective eyewear and disposable jacket. "I stand out," he admits.
The catchphrase of "flatten the curve" is all off, DiPaola says, because it assumes the health care system capacity is stable. But in reality, if teams of doctors and nurses are quarantined or fall ill, the health care system capacity will be greatly diminished. If one nurse tests positive, for example, 20 other health care employees she's been in contact with may immediately be quarantined, too.
"I don't know if I'm a carrier so I want to protect my patients," said DiPaola, who is the medical team leader of the organization www.endcoronavirus.org. "And I don't know which patient is positive and by the time we find out or even suspect, they could have contact with multiple personnel within the system. So my guiding principle is analogous to bloodborne universal precautions that we practice in the operating room: Assume everyone is positive and act accordingly."

Dr. Christian DiPaola always wears full protective gear in his Massachusetts hospital, going much further than CDC guidelines. (Contributed photo.)
Dr. Jason Adler, an emergency medicine doctor in Maryland and a husband and father of two, said frontline health care workers are grappling with their own mortality and their mental health.
Adler is worried about all levels of health care workers, from the lab technicians handling the COVID-19 swabs to the workers who clean up the hospital rooms after procedures.
“We're probably going to get infected. Some people will do better than others, but it's probably going to happen. As an ER physician, I think the likelihood is very high," Adler said.
CLICK HERE TO GET THE FOX NEWS APP
The ambiguity and uncertainty surrounding the virus have taken a toll and emotions can whip up at home, on social media and over email.
"I am concerned about the mental health of our front line health care workers," Adler said. "...We need a purge valve, and I'm concerned the front line workers, and many Americans, just don't have that right now.
"It's tough," he said. "We run into the fires and not away from them. But at the same time. It's very valuable to recognize that this is not normal."