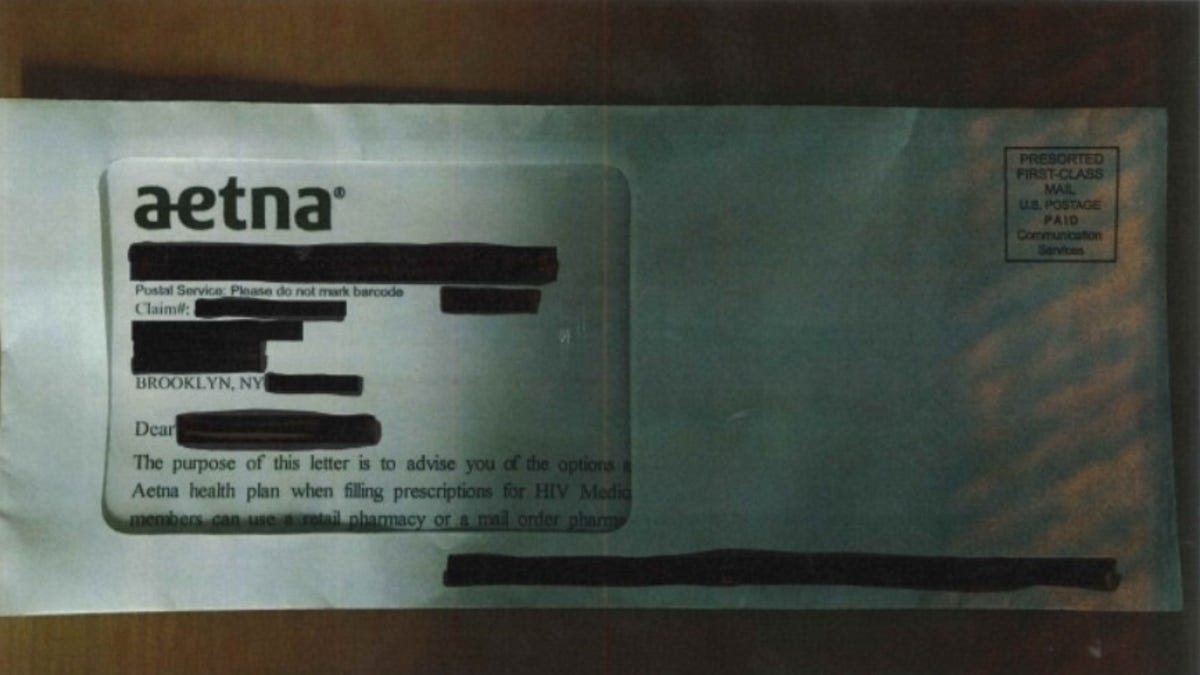
Aetna reportedly revealed the status of HIV patients when mailed envelopes showed personal data through a large window on the front. (Legal Action Center)
Aetna has reached a $17 million settlement after a class action lawsuit argued the health insurer breached the privacy of thousands of customers who take HIV medications.
Court documents state the company sent patients envelopes with large, clear display windows that revealed they were prescribed HIV medications.
AETNA REVEALED HIV PATIENTS' PERSONAL DATA, LEGAL GROUPS ALLEGE
The mailing, sent on July 28, was sent to about 12,000 customers in at least 23 states.
Aetna agreed in the settlement, which requires court approval, to pay at least $500 to customers whose privacy was breached through the revealing envelopes. The company also agreed to pay $75 to customers whose names were improperly disclosed to a mail vendor.

Aetna said in a statement the company is "implementing measures designed to ensure something like this does not happen again." (AP Photo/Jessica Hill, File)
Aetna said in a statement the company is working to remedy the situation.
“Through our outreach efforts, immediate relief program and this settlement, we have worked to address the potential impact on members following this unfortunate incident,” the statement read.
“In addition, we are implementing measures designed to ensure something like this does not happen again as part of our commitment to best practices in protecting sensitive health information,” the company stated, noting it’s taking steps to prevent other mishaps.
CVS TO BUY AETNA FOR $69 BILLION
The lawsuit originated in Pennsylvania with a 52-year-old Bucks County man whose sister learned he was taking HIV medications when she saw the Aetna letter mailed to him.
Aetna’s July mailing, according to a Legal Action Center press release, “was an attempt to address privacy concerns raised in two lawsuits filed against the insurer in 2014 and 2015.”
The Associated Press contributed to this report.








































