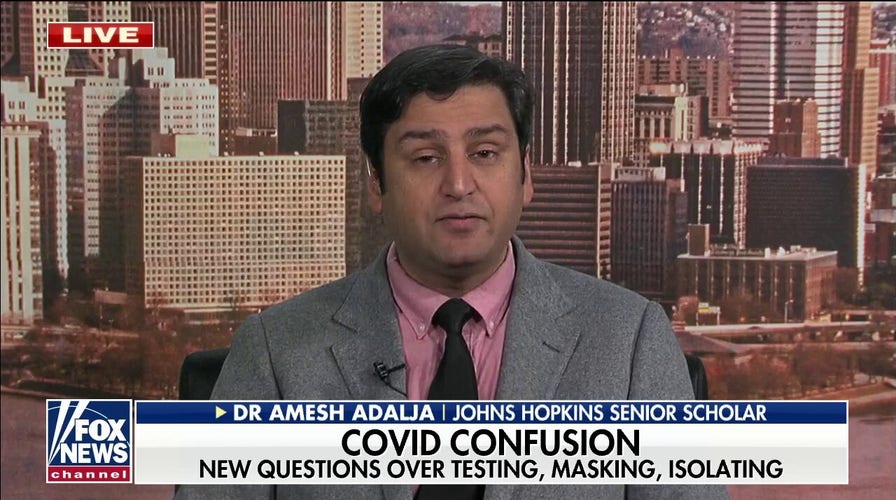
At-home COVID tests will help us live ‘sustainably’ with coronavirus: Infectious disease expert
Infectious disease expert Dr. Amesh Adalja joins ‘Cavuto Live’ to provide insight into the coronavirus pandemic.
Some health insurers say they will have trouble adapting to a new federal rule from the Biden administration requiring them to cover the costs of 8 at-home tests per month.
The rule, which takes effect this Saturday, requires private insurers to cover the costs of in-home tests but a New York Times report this week says that many insurers aren’t in a position to meet those requirements in the short term.

A health worker inoculates a boy with the CoronaVac vaccine, developed by China's Sinovac against the novel coronavirus disease COVID-19, at a vaccination centre in Bogota, on January 4, 2022, as the World Health Organization (WHO) warned that Omicron's dizzying spread increased the risk of newer, more dangerous variants emerging. (LEONARDO MUNOZ/AFP via Getty Images)
Insurers are saying it could take weeks to set up a proper system and pointing to the fact that over-the-counter tests are different from doctors visits and hospital stays that are typically covered.
The tests reportedly don’t have the type of billing codes needed for insurance to process claims and because health plans rarely process retail receipts it will force insurers to handle the cases manually at first.
BIDEN ANNOUNCES 500M MORE COVID TESTS TO BE DISTRIBUTED FOR FREE AMID OMICRON SURGE
"This is taking things back to the olden days, where you’ll have a person throwing all these paper slips in a shoe box, and eventually stuffing it into an envelope and sending it off to a health insurer to decipher," Ceci Connolly, president and C.E.O. of the Alliance of Community Health Plans, told the New York Times.

U.S. President Joe Biden listens while joining the White House Covid-19 Response Team's call with the National Governors Association discussing the Omicron variant in the Eisenhower Executive Office Building in Washington, D.C., U.S., on Monday, Dec. 27, 2021. Biden's medical adviser said a domestic travel vaccination rule should be considered as the omicron variant fuels record Covid-19 case loads in some states and holiday travel continues to be disrupted around the U.S. Photographer: Ken Cedeno/UPI/Bloomberg via Getty Images
Connolly added that the rule is being implemented too quickly as the rule was announced on Monday and supposed to take effect on Saturday.
"It is going to be exceedingly difficult for most health plans to implement this in four days," she said.
CLICK HERE TO GET THE FOX NEWS APP

Scientists at the Africa Health Research Institute in Durban, South Africa, work on the omicron variant of the COVID-19 virus Wednesday Dec. 15, 2021. The fast-moving omicron variant is complicating a key question: How does the COVID-19 pandemic end and the world co-exist with this virus? Experts agree that the coronavirus is here to stay. Ending the pandemic won't be like flipping a light switch. (AP Photo/Jerome Delay, File)
"There will be some people who buy them, and then have a six-month nightmare trying to get reimbursed," Jenny Chumbley Hogue, a Texas-based insurance broker, said about the rule adding that she has not yet seen a plan as to how the guidance will be handled.
Biden on Thursday directed health officials to purchase an additional 500 million COVID-19 tests to distribute to Americans for free, as the nation battles the surge in cases of the highly-transmissible omicron variant.
During remarks on his administration's strategy to address the COVID-19 pandemic, the president announced the additional 500 million tests – on top of the half a billion tests that his administration already has "in the process" of shipping to homes "for free."
The White House did not immediately respond to a request for comment from Fox News
Fox News' Brooke Singman contributed to this report