Colon cancer is the second leading cause of cancer-related deaths in the United States among cancers that affect both men and women— some 93,090 new cases are expected in 2015 alone. But there’s a good chance you don’t know the signs of colon cancer, how often you should be screened, or what puts you at a greater risk.
Knowing these basics and some of the lesser-known facts about colon cancer could help keep you and those around you healthy.
1. People frequently overlook colon cancer signs and symptoms.
When colon cancer is detected early, the survival rate is relatively high. But too frequently, the signs and symptoms are ignored.
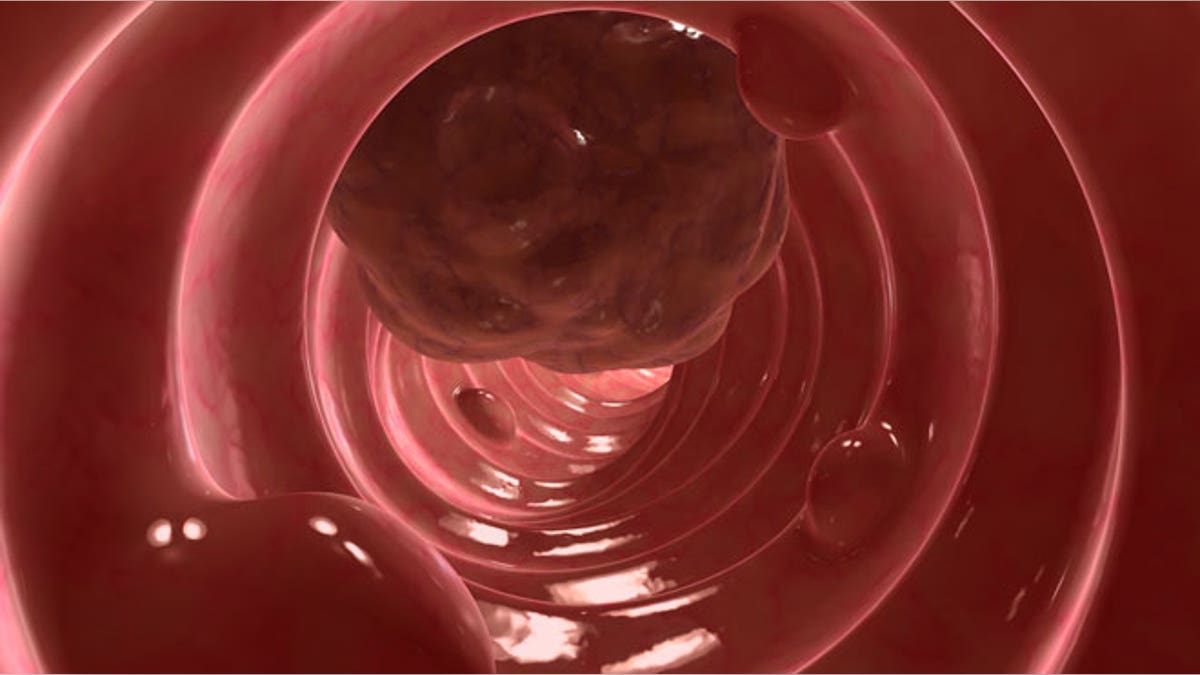
It can take 10 to 15 years for abnormal cells and new polyps to develop into colon cancer. This is ample lead time to identify and remove the growths. Colon cancer rates have fallen over the last 20 years, which is attributed largely to better screening practices— but still only about half of U.S. adults age 50 and older follow screening recommendations.
Although the American Cancer Society suggests regular colorectal cancer screenings begin at age 50, those with risk factors like a family history of the disease should speak with their doctors about starting annual screenings at an earlier age. Also talk to your doctor about any of the following symptoms, which could be signs of colon cancer:
• Blood in the stool
• Rectal bleeding
• Cramping, pain or chronic abdominal bloating
• Diarrhea, constipation or “narrow stools” that are outside of the norm for you and continue for more than a few days
• Feeling the urge to have a bowel movement, but not being relieved after doing so
• Unexplained weight loss, fatigue and weakness
READ MORE: How much does chemotherapy cost?
2. Your doctor may miss the signs.
Even if you identify the symptoms of colon cancer, there’s a risk you’ll be misdiagnosed. According to a 2014 study, one in 20 American adults are affected by a misdiagnosis. And though colon cancer misdiagnoses are relatively rare, affecting 0.007 percent of U.S. adults annually, the potentially fatal outcomes make the few diagnostic mistakes that do happen all the more important.
Research shows different diagnostic methods often have different results, and your doctor may simply misread a test result or underestimate the seriousness of your symptoms. If you have concerns about your diagnosis, or lack thereof, don’t be afraid to seek a second opinion.
READ MORE: This guide can help you find a second opinion.
3. Rates are higher and outcomes worse for certain populations.
Half of all premature colon cancer deaths are linked to disparities in race, education and geography, according to the American Cancer Society. Research has shown a higher incidence of death among colon cancer patients who are racial minorities, have only a high school education or less, or live in the South.
The research, which was published in the Journal of Clinical Oncology, suggests if all colon cancer patients experienced the lowest death rates of the most educated, white colon cancer patients, there would be nearly 8,000 fewer premature deaths every year nationwide.
READ MORE: Your colon cancer screening may be free under the ACA
4. Colon cancer risk is tied to red meat consumption.
Multiple studies have linked a higher incidence of colon cancer to a diet rich in animal proteins, and especially red meat. A 2005 European study that tracked 478,000 men and women found those who ate about five or more ounces of red meat per day were about 33 percent more likely to develop colon cancer. That same year, researchers in the U.S. found red and processed meat consumption to be linked to an increased risk of cancer, particularly colorectal cancer.
It’s important to note that these studies found correlations, not causation. In other words, they didn’t prove red meat causes colon cancer, merely that the two may be linked. On the other hand, a diet rich in vegetables, fruits and whole grains may help lower your risk, so redistributing portion sizes on your plate may be in order.
5. IBD and type 2 diabetes put you at increased risk.
If you suffer from inflammatory bowel disease (IBD) or type 2 diabetes, you are at a greater risk of developing colon cancer.
IBD includes Crohn’s disease and ulcerative colitis, two conditions that cause chronic inflammation of the colon. This inflammation can lead to dysplasia, or abnormal cells, that can become cancerous over time.
Likewise, people with Type 2 diabetes are at an increased risk. Much of this is due to shared risk factors for diabetes and colon cancer, like obesity, but even after accounting for these factors, the higher rate remains. The overall health of Type 2 diabetics also means that they have a worse prognosis once diagnosed with colon cancer.
For both of these diseases, officials recommend colon cancer screenings start earlier and happen more frequently.
Colon cancer is preventable
Many of the risk factors for colon cancer are within your control. From maintaining a healthy weight to eating right and watching for abnormal symptoms, you can reduce your risk of getting the disease, and increase the likelihood of a positive outcome thanks to early intervention. Even when you have a family history or a risk factor like IBD, regular screenings can identify polyps before they become cancerous.








































