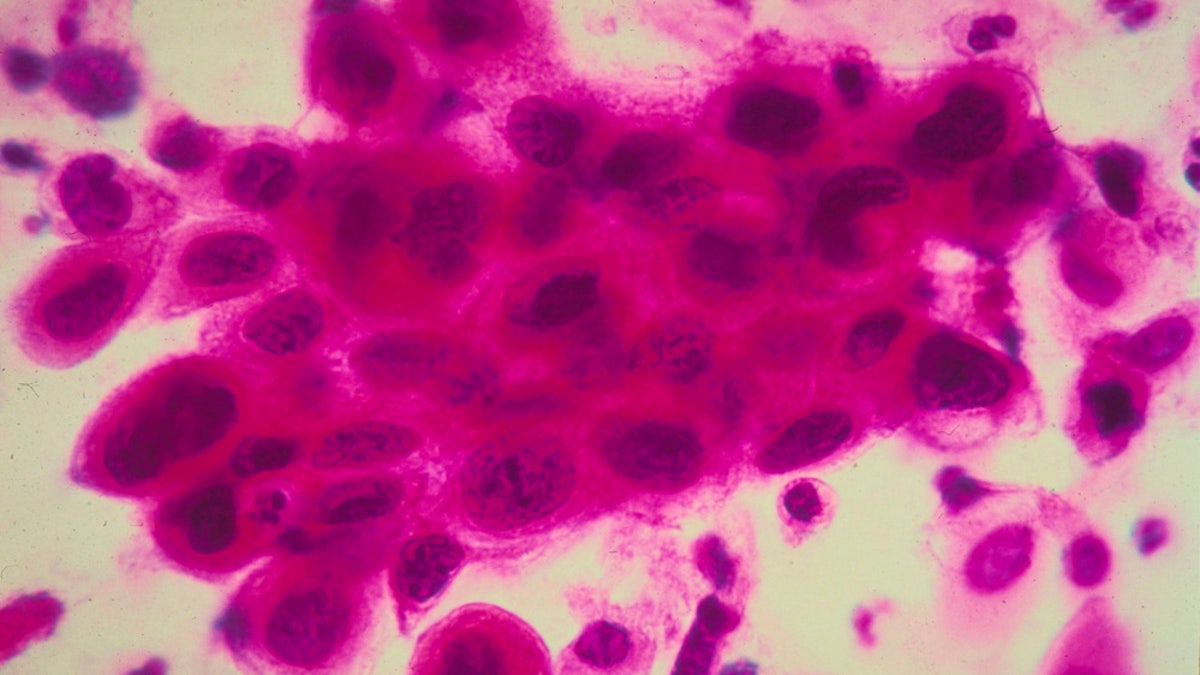
Close up of cancer cells in the cervix. Cancer of the uterine cervix, the portion of the uterus that is attached to the top of the vagina. (Photo by American Cancer Society/Getty Images)
In new interim guidelines released today, a panel of cervical cancer screening experts has recommended the human papillomavirus (HPV) test replace Pap tests for women as young as 25, AL.com reported.
According to the Centers for Disease Control and Prevention’s (CDC) latest data, 12,109 women in the U.S. were diagnosed with cervical cancer in 2011, while 4,092 women died from the disease that year. HPV is the most common sexually transmitted infection, affecting both men and women. Most infected persons do not realize they are infected or that they’re passing the virus to a sex partner.
Current guidelines from the U.S. Preventative Services Task Force use the Pap test as the primary tool for cervical cancer screening. Those guidelines advise that women ages 21 to 65 have the test done once every three years. Co-testing with the HPV test has been used for women age 30 and older. The combination allows patients to space out testing to once every five years if they take both tests.
"When you really look at it, the difference in performance between Pap tests and primary HPV is really quite impressive," lead panel author Dr. Warner Huh, senior scientist at University of Alabama at Birmingham Comprehensive Care Center, told AL.com. "Pap tests are missing a fair amount of clinically meaningful precancer."
In a separate study published in July 2014, researchers also found that HPV screening alone would be a viable alternative to Pap screening. Researchers used data from over one million women between ages 30 and 64.
Both tests study cells collected from the cervix. The cells are examined under a microscope for abnormalities in a Pap test, while an HPV test looks for the presence of human papillomavirus— specifically two types that are most likely to cause cancer. A positive test requires further examination, including a biopsy, to look for cancer or precancerous lesions.
Making the recommended change quickly may be difficult for physicians and their patients, Huh noted.
"For years, women's health care has been anchored around the Pap smear," Huh told AL.com. "Patients understand what a Pap smear is. Changing that is going to require some re-education."
While Pap tests have been the main tool for cervical cancer prevention for generations, there have been significant changes to it in the past 10 years, Dr. Eduardo Lara-Torre, a professor of obstetrics and gynecology at Virginia Tech Carilion School of Medicine, told AL.com. The test is no longer recommended annually, or for women older than 65 or younger than 21.
"In the past 10 years, we've really discovered more about the disease," Lara-Torre told AL.com. "And we've discovered that more Paps doesn't mean better outcomes."
While the latest guidelines have been implemented for a year, not all doctors— or patients— are following them, Lara-Torre said. He noted that some patients are reluctant to get screened every three years instead of annually because they are used to the more frequent screening.
Critics of the HPV test worry that there could be an overabundance of follow-up tests because not all HPV becomes cancer.
Human papillomavirus, an infection that usually clears up on its own, is common in teenagers and women in their 20s. Because of this, current guidelines call for HPV testing at age 30, the time when presence of the virus is more likely to lead to cancer, AL.com reported. Huh noted that the panel struggled with the recommendation to use the HPV test for women between ages 25 and 29.
"For women between the age of 25 and 29, the HPV test does substantially increase the number of [follow-up tests]," Huh told the news site. "But it also detects more clinically meaningful precancer. There is a price to pay, but we do wind up finding more cancer."
According to Huh, the HPV test provides more peace of mind than a Pap test because a negative result means the patient has a less than 1 percent chance of developing cancer in the next three years.
The panel made their recommendations based on a three-year study of the HPV test on 47,000 women. Huh noted it’s unlikely the official guidelines will change anytime soon, as the U.S. Preventative Services Task Force is likely to want more data.
Huh also noted that the Pap test is not going away. It is still the primary test for women in their early 20s and a follow-up test for some women with a positive HPV test. Both tests are protective for women of all ages not at risk of developing cervical cancer.
“The most important message is that women need to get screened," Huh told AL.com. "If women don't get screened, irrespective of the strategy, it will be hard for us to decrease the rates of cervical cancer."
The research was published simultaneously in the journals Gynecologic Oncology, Obstetrics & Gynecology, and the Journal of Lower Genital Tract Disease.
