A program that offered long-acting no-cost contraception to U.S. girls and women age 15 to 19 reduced the teenage pregnancy rate by 79 percent over five years and cut the abortion rate by 77 percent, according to the results of a new study.
"This has really important public health implications in the United States, where we have had persistent challenges in trying to decrease unintended pregnancy," said Cynthia Harper, a professor of obstetrics, gynecology and reproductive services at the University of California, San Francisco. She was not involved in the research.
"The findings were surprising because they had such a large impact," she told Reuters Health.
The report in the October 2 New England Journal of Medicine comes at a time when more than 600,000 U.S. teens become pregnant each year.
By age 20, about 20 percent of white teens and 40 percent of Hispanic and black teens will have been pregnant, according to The National Campaign to Prevent Teen and Unplanned Pregnancy.
The new study comes from the Contraceptive CHOICE Project conducted in the St. Louis area. It was designed to see if teen pregnancy rates could be brought down by aggressively providing information on contraceptives and offering contraception for free.
"For many years, parents, practitioners and policy makers thought, 'Those (long-acting contraception) methods aren't for teens; they're not going to want those methods.' We were able to demonstrate that if they are properly counseled and if they have a choice, they will pick those methods, actually use them, and have really great outcomes as a result," said chief author Gina Secura of the Washington University School of Medicine in St. Louis.
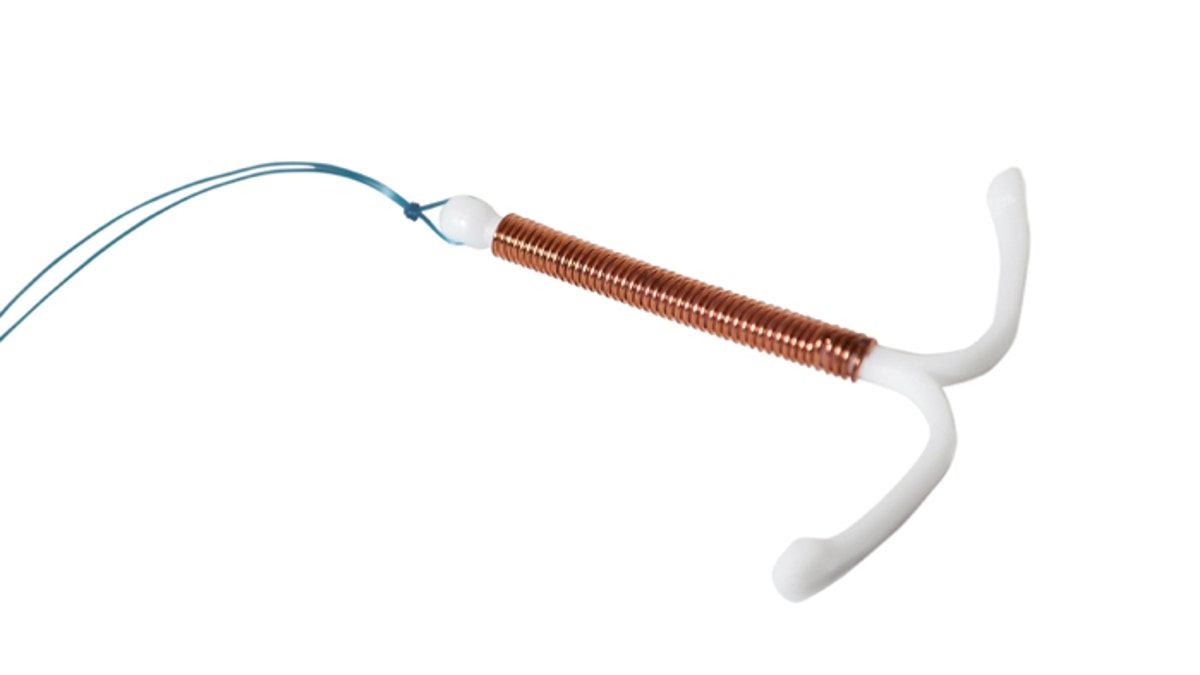
The teens, all of whom had sought contraceptive services through a clinic, were told about various types of birth control, including the long-term injectable and implantable contraceptives such as IUDs that have been used around the world for years and whose effects are reversible. Generally, fewer than 5 percent of U.S. teens use such methods.
Ultimately, 72 percent of the 1,404 teenage girls and women enrolled in the study went with an intrauterine device (IUD) or an implant. Only 12.5 percent opted for an oral contraceptive pill. The volunteers were followed for as long as three years during the study period, which lasted from 2008 to 2013.
The annual rate of pregnancy was 3.40 percent compared to 15.85 percent in a survey of sexually experienced U.S. teens and women in the same age group. The likelihood of giving birth each year was 1.94 percent among the St. Louis teens versus 9.40 percent nationally.
The abortion rate was 0.97 percent when the long-acting contraception was free, compared to 4.15 percent in the rest of the U.S.
"These methods are not known by teens and providers are not used to providing them," Harper said.
She said young women seeking contraception should initially ask their doctor which method is the most effective because - unlike doctor-patient discussions about other medical treatments - when it comes to contraception, "effectiveness is not always one of the things that is discussed."
"What we saw was that among the teens who started with the shorter-acting methods like the pill or the patch, after a while they started to see they were forgetting to use them. And they then transitioned to a long-acting method," Secura told Reuters Health.
The girls and women in the study were not new to sex. Nearly half had already had an unintended pregnancy, 18 percent reported having had at least one abortion and nearly three quarters reported having sexual intercourse during the 30 days before they enrolled in the study. Only 3 percent were sexually inexperienced.
When the researchers compared the young women in the study to all U.S. women - both sexually experienced and inexperienced - ages 15 to 19, they found that the program reduced the pregnancy rate by 41 percent, the birth rate by 44 percent and the abortion rate by 34 percent.
Secura said more teens and young adults are not using the longer-acting methods because, "Historically, it's been easier for practitioners to write a prescription for pills and have a teen go on her way."
In addition, inserting long-acting contraception devices "take more training than some family physicians are used to," Harper said.
The other problem: the longer-acting methods are far more expensive, at first.
"The up-front costs are anywhere from $500 to $1,000, depending on the device and the cost of the insertion," said Secura.
"You reach cost neutrality within two years with the long-acting methods. But these methods last three, four, five, or six years. So not only are they more effective, they start to regain the financial investment while they're still in use," she said.
"Hopefully, data like this can show people why it's so important to cover contraceptives for women's health," said Harper.




















