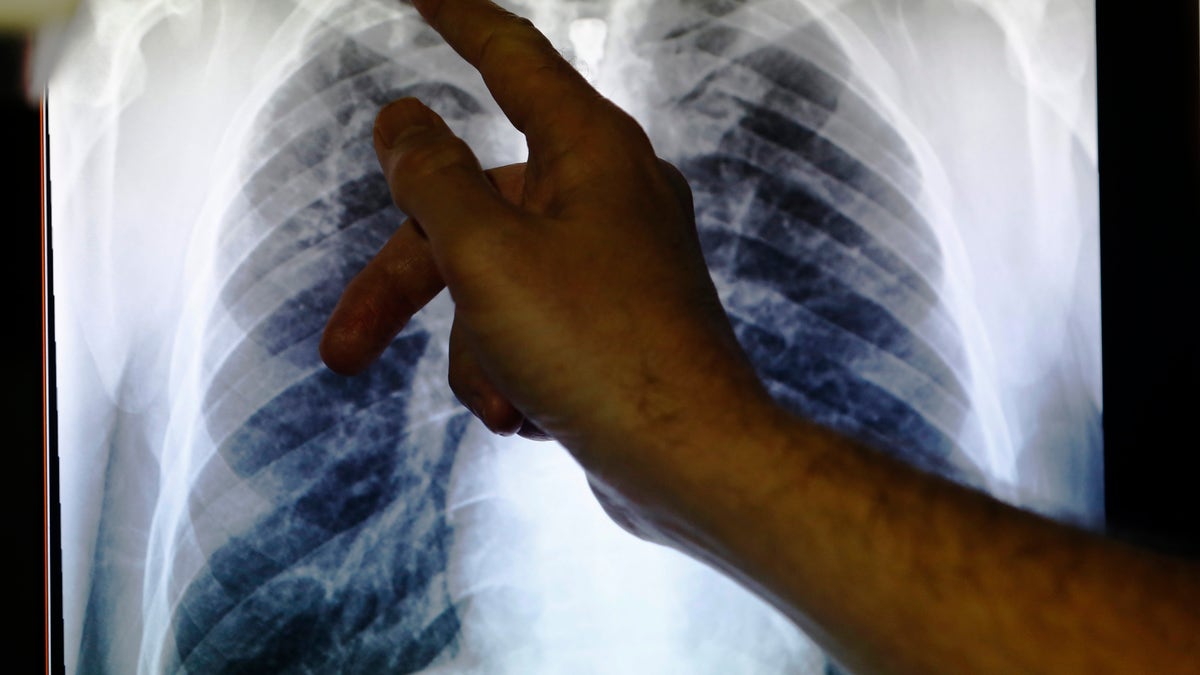
Jan 27, 2014 -Clinical Dr Al Story points to x-ray showing lungs infected with TB (tuberculosis) in London. (REUTERS)
The World Health Organization published new data this week revealing that tuberculosis has become the world's leading infectious killer. About 1.5 million people died from TB in 2014-surpassing the number of deaths caused by HIV/AIDS.
The announcement is likely to catalyze more aggressive efforts to expand access to TB treatment as a way to curb the epidemic. As efforts improve to expand TB treatment to everyone in need, it's critical that we ensure the quality of the medicines people receive through treatment programs.
Poor quality medicine presents an escalating challenge to public health efforts, especially in low- and middle-income countries. The problem is two-fold and includes both falsified medicines and substandard medicines. Falsified medicines are illegal or bogus medicines made by counterfeiters to appear to be legitimate medicines. Substandard medicines are superficially legal medicines that, when manufactured with poor quality control, means they fail to meet minimum quality requirements. In some instances, this may be a small regulatory violation, in others it can be criminal negligence.
As the number of people treated for TB increases, it becomes even more important to ensure that those medicines are of good quality. Evidence from my team's empirical research and published in the peer-reviewed literature shows this is not always the case. For TB, which is caused by a bacterial infection, taking poor quality medicines not only creates risks for the patient-who might die as a result-but also creates risks for the broader community through the emergence of drug resistance. Studies have shown that substandard drugs are likely contributing to the development of multidrug-resistant TB, which is deadlier and far more expensive to treat-- up to $400,000 per infection compared with under $1,000 on average for standard TB.
Pharmacovigilance isn't optional or nice to have. It is a fundamental component of health care. With two new medicines for drug-resistant TB recently approved and a new international effort to end TB underway, ensuring the quality of treatments is paramount.
One of the strongest tools we have to ensure drug quality is called pharmacovigilance. This is the practice of monitoring, understanding and responding to adverse reactions to medicines once they have been licensed for use and have made their way to patients.
Pharmacovigilance is an essential and routine function of modern healthcare systems. Unsurprisingly, these activities are also expensive. In Europe, for example, the estimated cost of fees to monitor and conduct safety reports can exceed $300,000 per medicine. In low-income countries where TB hits hardest, however, pharmaceutical manufacturers and governments alike often see these costs as prohibitive.
The campaign to improve access to medicines for people living in poverty has gained extraordinary momentum in the last decade. The resulting improvement in access to treatment has not been accompanied, however, by commensurate efforts to ensure the quality of that treatment. Efforts have predominantly focused on distributing medicines as quickly and cheaply as possible, with relatively less emphasis on ensuring the quality of medicines or the integrity of the supply chain. Whether this is attributable to limited knowledge or limited resources, the result is the same: more drugs without a commensurate strengthening of oversight. In many nations across Latin America, Africa and Asia, regulations for pharmacovigilance exist but are never followed.
Some programs, such as President Obama's Malaria Initiative, and the Geneva-based Global Fund to Fight AIDS, Tuberculosis and Malaria, and some TB-affected country governments such as Rwanda do meet basic pharmacovigilance requirements. But these efforts pale in light of the scale of programs and the vast, unmet need elsewhere.
This needs to change. Pharmacovigilance isn't optional or nice to have. It is a fundamental component of health care. With two new medicines for drug-resistant TB recently approved and a new international effort to end TB underway, ensuring the quality of treatments is paramount.
