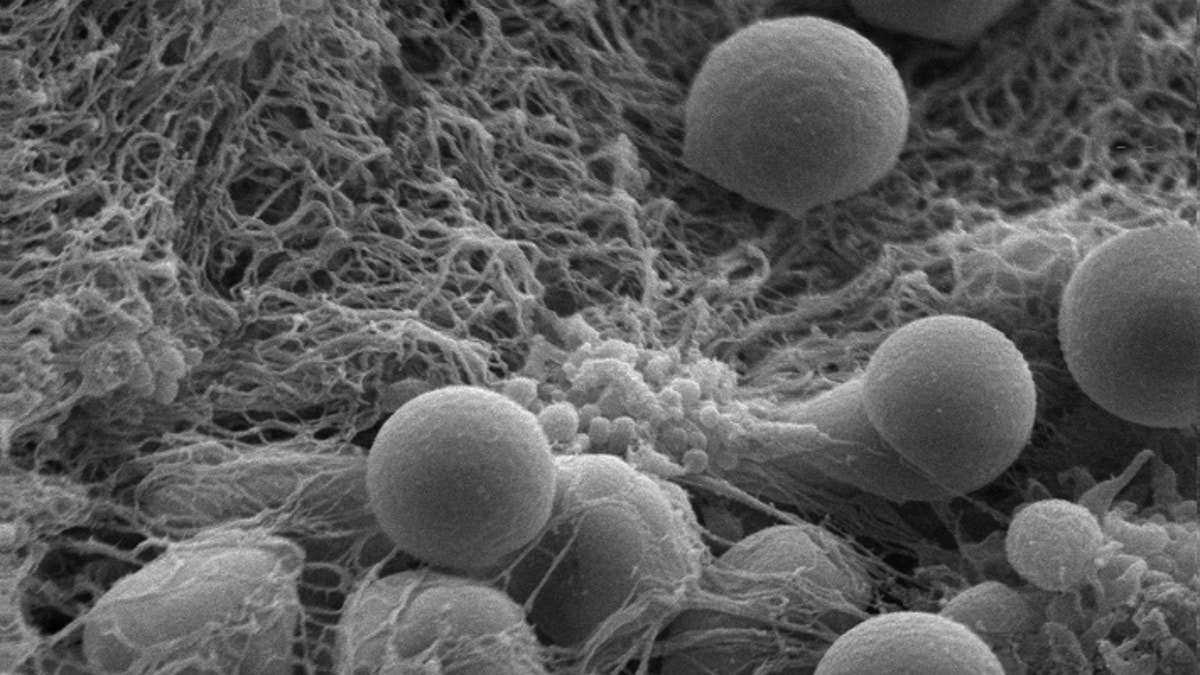
Hemostatic nanoparticles accumulate on a clot-stabilizing mesh of fibrin the body produces. (Andrew Shoffstall)
For soldiers exposed to powerful bomb blasts or victims of severe car accidents, the timing of treatment is critical for survival. Such traumas can lead to uncontrolled internal bleeding, and if blood transfusions are not given in time, these injuries are often fatal.
But now, there may be a quick fix for these types of wounds that could potentially save thousands of lives. In a new study published in the Proceedings of the National Academy of Sciences, researchers developed and tested a type of artificial platelet, which can be injected into the body and spur the faster formation of blood clots.
These nanoparticles could drastically slow down internal bleeding, giving patients enough time to seek proper medical attention. According to the researchers, such a solution is critical given the lack of treatments available for this dangerous type of injury.
“We were doing research on the effects of internal injuries on other [organs], and we couldn’t find anything that worked to stop internal bleeding,” study author Erin Lavik, an associate professor of biomedical engineering at Case Western Reserve University in Cleveland, told FoxNews.com. “It’s still shocking that we don’t have something…Right now, when you have a trauma and internal bleeding, the most common treatment is to get transfusion of blood products, but they’re not particularly effective if you have massive bleeding.”
Lavik and fellow researchers at Case Western Reserve, Wayne State University and Virginia Tech decided to team up and create their own solution to this problem. The result: their newly developed hemostatic nanoparticles made from short polymer chains and peptides. According to Lavik, these tiny particles help to speed up the body’s natural clotting process.
During internal hemorrhaging, the body’s platelets – blood cells whose purpose is to stop bleeding – are activated and bind together to form clots. Yet sometimes the internal bleeding is too extensive, and there are not enough natural resources to stop the loss of blood. These nanoparticles help to fix this problem by acting like tiny bridges, connecting the body’s activated platelets so that more and more cells can band together and form stronger blood clots.
Additionally, the nanoparticles do not interfere with the natural healing process or form free-floating clots that could cause deadly strokes.
“We purposefully made it out of biodegradable material, so they don’t last too long in the body, and we made them small,” Lavik said. “The particles are about 500 nanometers so it’s about 1/200 of the thickness of a human hair. They’re tiny, and we did that because we didn’t want the particles themselves to trigger clotting.”
To gauge their invention’s effectiveness, the researchers tested their nanoparticles in mice models of blast trauma. When injected into the mice with traumatic injuries, the particles increased survival rates to 95 percent, compared to only 60 percent in the untreated mice. And the injected mice remained healthy up to several weeks post-injection, indicating successful long-term survival.
“We can track them out to a week after trauma,” Lavik said. “The really important thing is…your clot has to be stabilized by a fibrin mesh web, and these particles don’t inhibit that web formation. We form stable clots that stay stable.”
According to researchers for Veterans Affairs hospitals, blast exposure accounts for 79 percent of all combat-related injuries, and it is the leading cause of death on the battlefield. Additionally, the risk of traumatic injury isn’t just overseas, as uncontrolled bleeding from car accidents, blows and falls is one of the leading causes of death among Americans, according to the Centers for Disease Control and Prevention.
Along with using blood products to stem bleeding, hospitals can also use a hemophilia medicine called recombinant factor VIIa. However, the medication must be refrigerated in order to be effective and can cause clots in the brain and spinal cord injuries. Lavik and her team’s nanoparticles remain viable for up to two weeks on the shelf. Ideally, a medic in the field would just need to add saline and shake the solution before injecting it into a trauma victim.
“Hopefully, if everything goes well, and they’re safe and effective in humans, we’d love to have something that can be in a paramedic’s bag and can be administered as quickly as possible after trauma,” Lavik said. “The earlier you intervene, the better the outcome.”
