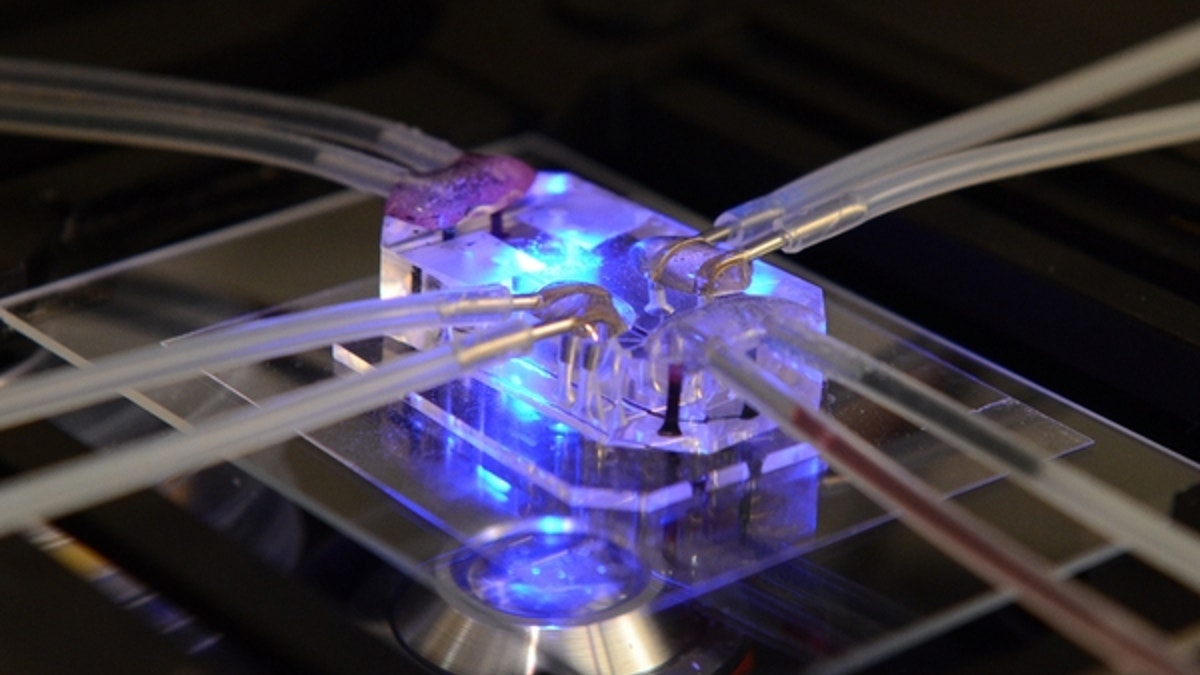
This plastic device, which is about the size of a flash drive, mimics the function and one of the illnesses of a human lung. (Courtesy Wyss Institute, Harvard University)
This fingertip-size device can't exactly cough, but it can get a lung disease. For the first time, researchers have reproduced some of the effects of a disease in a microchip. The scientists' "organ-on-a-chip" technology is still under development, but they hope it someday will help test therapeutic drugs more quickly and reliably than current methods allow.
"There's a huge need to find more predictive alternatives" to the lab mice that pharmaceutical companies rely on now, said Geraldine Hamilton, who worked on the diseased lung-on-a-chip. Hamilton manages the organs-on-a-chip research program at Harvard University's Wyss Institute. "We think that the organs on chips truly provide that alternative," she told TechNewsDaily.
Organs-on-a-chip are plastic microchips designed to act as small, simplified versions of lungs, hearts and other bodily organs. Unlike the microchips in computers, they don't have circuits imprinted on them. Instead, they're etched with tiny channels that carry water, air, blood or other biological fluids. The channels are lined with living cells taken from either rats or humans, to help them act more like real organs.
The researchers who make them hope they'll become more-accurate testing grounds for drugs than lab rats, or simple collections of cells grown in a Petri dish, are. The vast majority of newly invented treatments that work well in lab mice don't ultimately work in people.
"What happens is the drugs fail when they get to these much later stages, either when they reach clinical trials or even after they get to market," Hamilton said. That costs drug companies time and money, she said. She and other organs-on-a-chip researchers hope better tests for potential drugs will help labs discover early on which drugs work and which don't.
U.S. research agencies are investing heavily in organs-on-a-chip tech. The National Institutes of Health plans to give U.S. labs as much as $70 million over five years to develop the chips. The NIH has signed an agreement to give as much as $37 million to the Wyss Institute alone.
In the latest step forward in organs-on-a-chip research, Hamilton and her colleagues re-created a lung condition called pulmonary edema, or fluid leakage into the lungs. Hamilton worked with researchers from Harvard, Children's Hospital Boston and the drug company GlaxoSmithKline.'
The lung-on-a-chip had two channels, designed to represent an air sac in the lung and an adjacent blood vessel. Hamilton's team even hooked a tiny vacuum up to chip. The vacuum stretched and released the chip's "lung" channel as if it were an air sac in a working lung, expanding and deflating with every breath.
To give the chip pulmonary edema, the researchers injected a chemotherapy drug, interleukin-2, into the "blood vessel" channel. Pulmonary edema is a potentially fatal side effect of interleukin-2, also known as IL-2, which treats skin melanomas and kidney cancer. In the lung microchip, researchers used the same doses of interleukin-2 that human patients get, on the same time schedule.
The IL-2 injection caused fluid to leak from the lung-on-a-chip's blood vessel channel into the lung air sac channel. It also caused blood clots to form in the air sac channel. Such fluid leakage and clot formation also happen in pulmonary edema in people.
The lung-on-a-chip researchers discovered something along the way: They found that the vacuum-created "breathing" action of the chip actually increased the fluid spillage in the chip. "We didn't expect that mechanical breathing motions would be responsible for the large majority of the edema produced by IL-2," Hamilton said.
It will be a long time yet before plastic chips replace lab rats and Petri dishes in drug labs. "We are beginning the validation process," Hamilton said. Wyss scientists are now starting to talk with pharmaceutical companies and regulatory agencies about what experiments they want to see before they would feel confident about using chips instead of lab animals, Hamilton said.
When the technology is ready, however, Hamilton and her colleagues imagine it could test much more than therapeutic drugs. It could test the safety of cosmetics, pollutants or food, she said. It could also teach researchers more about diseases, such as pulmonary edema.
Hamilton and her team published their work Nov. 7 in the journal Science Translational Medicine.
- Bionic Humans: Top 10 Technologies
- 3D-Printed Sugar Technique Makes Artificial Blood Vessels
- 10 Sci-Fi Predictions That Came True
Copyright 2012 TechNewsDaily, a TechMediaNetwork company. All rights reserved. This material may not be published, broadcast, rewritten or redistributed.
