Reading an insurance policy may seem like reading a foreign language, but that’s no excuse to file it and forget it - or worse, to skip getting insurance altogether.
According to the World Health Organization, 64 million women in the U.S. suffer from at least one of the “Big 6” health conditions - heart disease, cancer, hormone disorders, diabetes, joint conditions and mental health issues. The bottom line? We all need health insurance. That’s why I decided to call in an expert to help translate the insurance lingo and decipher what everyone should understand about their own policy.
Dr. Archelle Georgiou is a healthcare executive and former Chief Medical Officer of United Healthcare. Here are some key points she explained to me:
Health insurance cannot be customized
That means if you buy an individual policy, you can’t pick and choose your benefits to build the policy you want. By law, insurance companies must file exactly what’s in their policies with the state. To offer some choices, an insurance company might file several different policies with slightly different benefits in a particular state. Any options within the plans must be listed in the filing.
It’s similar to buying a car. If a car comes with black or gray seat fabric, those are your choices. You can’t order a car with blue seats. The same is true even when employers buy health insurance for their employees. If MyBoss decides to have HealthPick as the company's insurance carrier, MyBoss has to choose between the plans that HealthPick filed with the state.
Read the ‘exclusions’ section
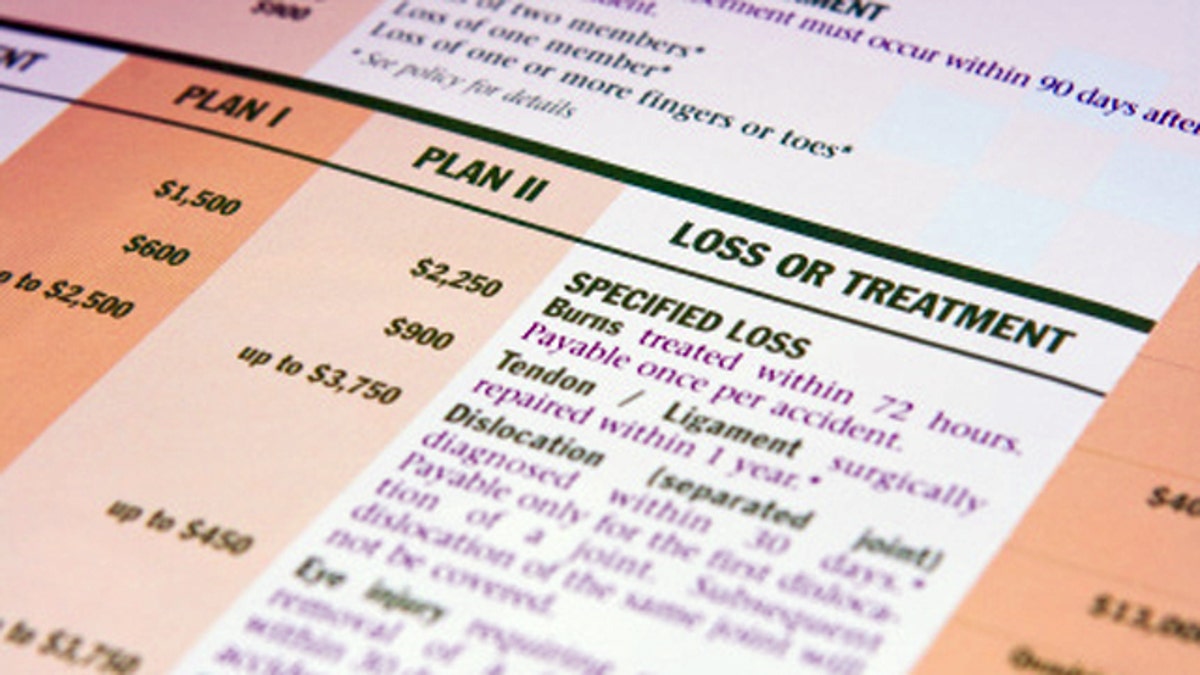
Exclusions are health care services that are specifically not covered by the policy you choose. Keep in mind that your health insurance policy is a contract. In the exclusions section, the insurance company is telling you in advance that it will not pay for certain things. Exclusions may be for very specific treatments – such as in vitro fertilization or acupuncture – or they can be for broader categories like maternity care.
Another common exclusion is mental health care coverage. The Centers for Disease Control and Prevention reported that one out of four adults are affected by depression and estimated that by the year 2020, depression will become the second highest cause of disability for men and women around the world. That shows how significant mental health care coverage could become, even if you don’t see a need for it right now. The important thing is to make sure you know what your policy says before planning any treatments so you won’t be surprised by a claim that is denied.
Understand ‘Out of Network’ providers
‘Out of Network’ means the doctor or facility does not have a contract with your insurance company. If your insurance covers Out of Network providers, the policy will explain what is covered. For example, my HealthPick policy may state that it covers 60 percent of the “usual and customary” fees for Out of Network providers. The trick is knowing what “usual and customary” means.
Here’s an example: Dr. X is an Out of Network provider. He charges $10,000 to take care of me. HealthPick will cover 60 percent of what is “usual and customary.” That doesn’t necessarily mean HealthPick will pay $6,000 for the treatment. HealthPick might say that what is “usual and customary” is only $5,000 for that treatment. Sixty percent of $5,000 means HealthPick will only pay $3,000 of coverage.
Since Dr. X is an Out of Network provider, he does not have a contract with HealthPick, so he does not have to accept what they are willing to pay. Because I chose to go to Dr. X, I created a contract directly between Dr. X and myself. So I owe Dr. X the additional $7,000 that HealthPick did not cover. Using an Out of Network provider can be very expensive, even if your policy has Out of Network coverage. In the example I just gave, if my policy didn’t cover Out of Network providers at all, I would have to pay the entire $10,000 with no help from my insurance.
Health insurance can be a lifeline to protect your family and your finances. Take the time to shop around to find a policy that fits your needs. It’s up to you to decide which policy is the right fit for you and your family. Most importantly, read the fine print before you need to use your insurance. You are responsible for knowing how to use your insurance, the rules you have agreed to follow, and what is covered.
